Depression is highly prevalent in hospice and palliative care settings—especially among cancer patients, in whom the prevalence of depression may be 4 times that of the general population.1 Furthermore, suicide is a relatively common, unwanted consequence of depression among cancer patients.2 Whereas the risk of suicide among advanced cancer patients may be twice that of the general population,3 in specific cancer populations (male patients with pancreatic adenocarcinoma) the risk of suicide may be 11 times that of the general population.4
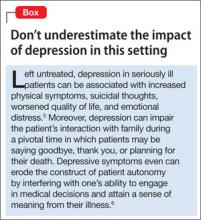
Mental health professionals often are consulted when treating depressed patients with advanced illness, especially when suicidal thoughts or wishes for a hastened death are expressed to oncologists or primary care physicians. To mitigate the effects of depression among seriously ill patients (Box),5,6 mental health professionals must be able to assess and manage depression in patients with progressive, incurable illnesses such as advanced malignancy.
Diagnostic challenges
Assessing depression in seriously ill patients can be a challenge for mental health professionals. Cardinal neurovegetative symptoms of depression, such as anergia, anorexia, impaired concentration, and sleep disturbances, also are common manifestations of advanced medical illness.7 Furthermore, it can be difficult to gauge the significance of psychological distress among cancer patients. Although depressive thoughts and symptoms may be present in 15% to 50% of cancer patients, only 5% to 20% will meet diagnostic criteria for major depressive disorder (MDD).8,9 You may find it challenging to determine whether to use pharmacotherapy for depressive symptoms or whether engaging in reflective listening and exploring the patient’s concerns is the appropriate therapeutic intervention.
Side effects from commonly used therapeutics for cancer patients—chemotherapeutic agents, opioids, benzodiazepines, glucocorticoids—can mimic depressive symptoms. Clinicians should include hypoactive delirium in the differential diagnosis of depressive symptoms in cancer patients. Delirium is an important consideration in the final days of life because the condition has been shown to occur in as many as 90% of these patients.10 A mistaken diagnosis of depression in a patient who has hypoactive delirium (see “Hospitalized, elderly, and delirious: What should you do for these patients?” page 10) might lead to a prescription for an antidepressant or a psychostimulant, which can exacerbate delirium rather than alleviate depressive symptoms.
Significant attitudinal barriers from both clinicians and patients can lead to under-
recognition and undertreatment of depression. Clinicians may believe the patient’s depression is an appropriate response to the dying process; indeed, feeling sad or depressed may be an appropriate response to bad news or a medical setback, but meeting MDD criteria should be viewed as a pathologic process that has adverse medical, psychological, and social consequences. Time constraints or personal discomfort with existential concerns may prevent a clinician from exploring a patient’s distress out of fear that such discussions may cause the patient to become more depressed.11 Patients may underreport or consciously disguise depressive symptoms in their final weeks of life.12
Responding to these challenges
The Science Committee of the Association of Palliative Medicine performed a thorough assessment of available screening tools and rating scales for depressive symptoms in palliative care. Although the committee found that commonly used tools such as the Edinburgh Depression Scale and the Hospital Anxiety and Depression Scale have validated cutoff thresholds for palliative care patients, the depression screening tool with the highest sensitivity, specificity, and positive predictive value was the question: “Are you feeling down, depressed, or hopeless most of the time over the last 2 weeks?”13,14
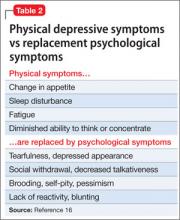
Other short screening algorithms have been validated among palliative care patients (Table 1).15 Endicott proposed a structured approach to help clinicians differentiate MDD from common physical ailments of progressive cancer in which physical criteria for an MDD diagnosis are substituted by affective symptoms (Table 2).16 The improved risk-benefit ratio of selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), coupled with the potential significant morbidity associated with MDD and subsyndromal depressive symptoms, makes it necessary to recognize and treat those symptoms even when the cause of the depressive symptoms is unclear.
Psychotherapy in palliative care
Psychotherapeutic interventions such as dignity therapy, which invites patients to utilize a meaning-centered life review to address his (her) existential concerns, may help depressed palliative care patients.17 Evidence suggests a strong association between diminished dignity and depression in patients with advanced illness.18 Individualized psychotherapeutic interventions that provide a framework for addressing dignity-related issues and existential distress among terminally ill patients could help preserve a sense of purpose throughout the dying process. Surveys of dignity therapy have been encouraging: 91% of participants reported being satisfied with dignity therapy and more than two-thirds reported an improved sense of meaning.18