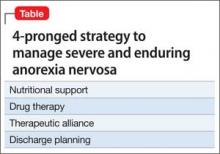
Severe and enduring anorexia nervosa (SE-AN) is persistent anorexia nervosa (AN) lasting for ≥7 years with or without a history of treatment. Evidence points to the effectiveness of a patient-tailored plan for treating SE-AN over any universal fix. Proper medication, therapeutic alliance, and strategic discharge planning are the ingredients for treating SE-AN that avoids re-hospitalization (Table).
Nutritional support and pharmacotherapy required
Comprehensive metabolic analysis and initiating nutrition should be the first priority for the medical team. Starved-state patients can have electrolyte and metabolic derangements that place them at risk of fatal arrhythmias or multi-system organ failure. Do not hesitate to initiate nasogastric tube feeding under the observation of a certified nutritionist when necessary for survival. A double-blind, randomized controlled trial demonstrated the benefit of olanzapine compared with placebo to increase body mass index (BMI) of hospitalized AN patients. Olanzapine was titrated from 2.5 to 10 mg/d over a 13-week period, and was associated with higher patient achievement of a BMI > 18.5 kg/m2.1
Although the patient is receiving nutritional support in conjunction with psychotropic medication, the road to BMI recovery can be long. Don’t forget that SE-AN can be incapacitating. In SE-AN, the fear of gaining weight is so severe that the idea of starvation-induced death initially might seem more palatable. Although counterintuitive, as the patient recovers metabolically, self-image deteriorates. Statements praising any new weight gain can derail any therapeutic relationship.
Therapeutic alliance is key
Establishing high-quality therapeutic alliance, as measured by the Helping Relationships Questionnaire, has been shown to have a positive outcome on eating disorder symptoms and comorbid depressed mood in later phases of SE-AN treatment.2,3 Although therapeutic alliance is individualized, maintaining open communication and reiterating how it is the patient’s decision to consume whole food at a level at which the feeding tube can be discontinued are good places to start treatment.
Proper discharge timing and transition to outpatient care for SE-AN patients is paramount. In multicenter studies, treatment ends too early in 57.8% of patients; discharge at sub-ideal BMI is linked to rehospitalization.3 Slower weight gain and delayed establishment of therapeutic alliance are predictors of patients who exit treatment programs too early.3 Clinicians who remain vigilant for the above metrics are less likely to feed into the unacceptably high rate of treatment failure for SE-AN.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.