Maximizing productivity is prudent for outpatient subspecialty clinics to improve access to care. The outpatient dermatology clinic at Parkland Health and Hospital System in Dallas, Texas, which is a safety-net hospital in Dallas County, decreased wait times for new patients (from 377 to 48 days) and follow-up patients (from 95 to 34 days) from May 2012 to September 2015.1 Changes in clinic productivity measures that occur with decreased wait times are not well characterized; therefore, we sought to address this knowledge gap. We propose that decreased wait times are associated with improvement in additional clinic productivity measures, specifically decreases in nonattendance and cycle times (defined as time between patient check-in and discharge) as well as increases in referrals.
In our retrospective cohort study of patients seen in the Parkland outpatient dermatology clinic between fiscal year (FY) 2012 and FY 2015 (between October 2011 and September 2015), we collected data on patient nonattendance rates, cycle times, and referral volumes. Categorical variables were compared using χ2 tests, and changes in cycle times were analyzed using 2-way analysis of variance. P<.05 was considered statistically significant.
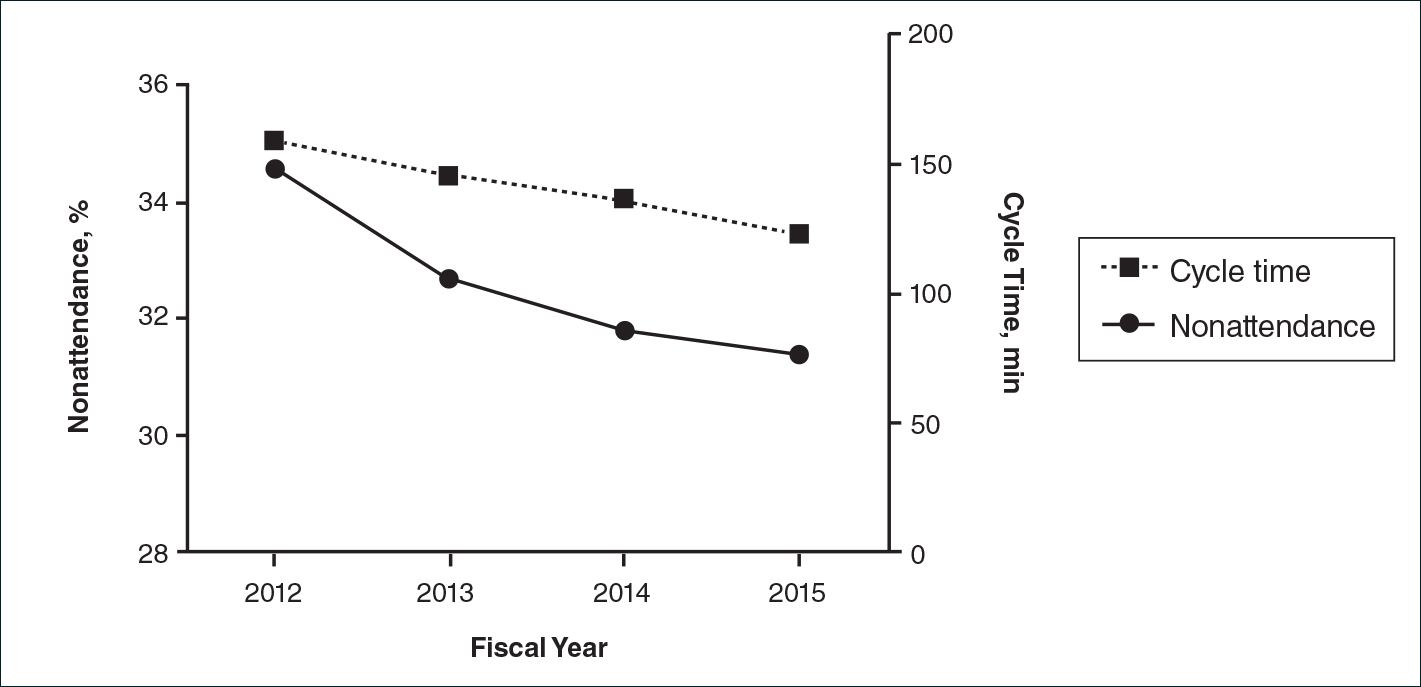
There were 52,775 scheduled clinic visits from FY 2012 to FY 2015. The overall proportion of patient nonattendance rates decreased from 34.6% (4202/12,141) to 31.4% (4429/14,119)(P<.001)(Figure), despite an increase in completed patient visits during the study period (7939 vs 9690). New patient nonattendance rates decreased from 42.9% (1831/4269) to 30.2% (1474/4874)(P<.001). The number of completed visits for new patients increased from 2438 in FY 2012 to 3400 in FY 2015. Follow-up nonattendance rates increased from 30.1% (2371/7872) to 32.0% (2955/9245)(P<.001). Follow-up completed visits increased from 5501 in FY 2012 to 6290 in FY 2015. Overall, average cycle time showed a trend to decrease from 159 to 123 minutes (22.6%)(Figure). Average cycle times were reduced from 159 to 128 minutes (19.5%) for new patients and from 161 to 115 minutes (28.6%) for follow-up patients (P=.02). Overall, referrals increased by 14.1% (816/5799)(P<.001), which was largely due to the increase in volume of referrals observed between FY 2014 (n=5770) and FY 2015 (n=6615).
We have demonstrated that decreased wait times can be associated with improvements in clinic productivity measures, namely decreased nonattendance rates and cycle times and increased referrals. Patient nonattendance is a burden on clinic resources and has been described in the dermatology clinic setting.2-6 Increased likelihood of nonattendance has been associated with prolonged wait times.3,7 We propose that decreased wait times can lead to diminished nonattendance rates, as patients are more likely to keep their appointments rather than seek other providers for dermatologic care. The difference in trends between new patient and follow-up nonattendance rates may be attributed to the larger relative increase in completed new patient visits compared to follow-ups during the study period.
Furthermore, the decrease in average cycle time reflected our clinic’s ability to see a larger number of patients per clinic, with subsequently shorter wait times. The greater reduction in cycle times for follow-up patients may be attributed to the increased continuity of providers who had previously seen these patients. Although the cycle times may seem high in our clinic compared to other practice settings, we believe that this marker of productivity is widely applicable to various clinic settings, including private practices and other outpatient specialty clinics. Increased clinic referrals can be a downstream effect of decreased wait times due to improvements in access to care, as shown in other specialty clinics.8 Effects of confounding variables on referral volumes, including nationwide health insurance changes during our study period, could not be ruled out.
Limitations of this study include unavailable data on patient and provider satisfaction and changes in patients’ health insurance. This study provides evidence of changes in clinical productivity measures associated with decreased wait times that can demonstrate widespread benefits to the health system.
Acknowledgments
The authors would like to thank Michael Estabrooks, RN, and Trung Vu for providing aggregate data, as well as Linda Hynan, PhD, for statistical advice (all Dallas, Texas).