Of course, there is a new final rule every year, so it really isn’t very final. I know this is confusing to many of you, I was dazed for several days by this year’s proposed final rule.
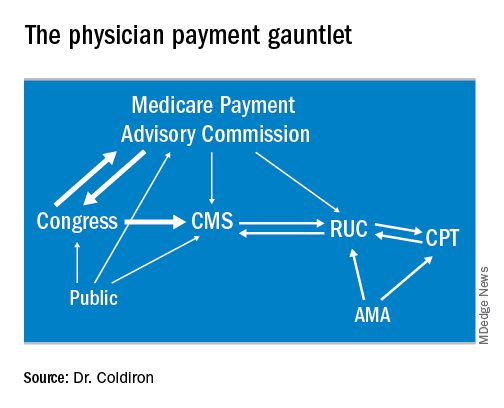
Each year, the Centers for Medicare & Medicaid Services receives input from innumerable sources and formulates its payment for physicians. These responses are often in response to requests by CMS itself, which wants to make sure reimbursements are accurate. Generally, input comes from the American Medical Association’s RVS Update Committee (RUC), which values new and existing CPT codes, as well as Congress, the Health & Human Services Office of Inspector General, lobbyists, specialty society organizations, public advocacy groups, and anyone who can wrangle an appointment at or write a letter to CMS headquarters in Baltimore. This conflicted brew is hashed over, and published in late July as a proposed rule. Public comments are then solicited (all letters and emails are considered, dermatologists sent 1,500 responses to this one!) and a final rule is published in the fall. I have constructed a flowchart of this process.
This year’s proposed rule was particularly disturbing because of major changes in reimbursement proposed by CMS. As you may recall, officials proposed to collapse all the evaluation and management (E/M) codes into two levels and pay bonuses to certain specialists (but not dermatologists). This might have been agreeable, except Medicare reimbursements are a zero-sum game. If someone is paid more, someone else will be paid less. Of course, you could always let the increase come out of the general pool, but that would decrease the conversion factor, and some health care professionals (usually primary care) might not see an overall increase. So, the proposed rule was going to “pay” for this increase by way of eliminating the 25 modifier, the CPT modifier that allows you to be paid for the evaluation and management (E/M) service on the same day as a procedure. This has been averted, at least for two years.
The final rule also makes a real effort to eliminate some meaningless documentation. Effective Jan. 1, 2019, for established patients, practitioners can focus their notes on patient changes. With new and established patients, they need not personally reenter the chief complaint and history already recorded by staff or the patient, other than simply indicate that they reviewed and verified the information in the medical record. In addition, teaching physicians do not have to duplicate notations by residents. CMS also included practice expense for additional skin biopsies.
CMS is also going to pay for services using communication technology. These include:
- Brief communication technology-based service, e.g. virtual check-in (HCPCS code G2012). This is provided by a physician or other qualified health care professional who can report E/M services for an established patient, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion. It is important to note that CMS is allowing for this code to include audio-only, real-time telephone interactions, in addition to synchronous, two-way audio interactions that are enhanced with video or other kinds of data transmission.
- Remote evaluation of recorded video and/or images submitted by an established patient (HCPCS code G2010). This is remote evaluation of recorded video and/or images submitted by an established patient (e.g., store and forward), including interpretation with follow-up with the patient within 24 business hours, not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment). The code can be reported effective Jan. 1, 2019, for established patients only.