Case Letter

Psoriasis and Leprosy: A Mystifying Coexistence
Psoriasis and leprosy exist mutually exclusively with only a few cases being reported regarding their coexistence. Among the various forms of...
From Dicle University, Diyarbakır, Turkey. Drs. Harman, Uçmak, and Akkurt are from the Department of Dermatology, and Dr. Türkçü is from the Department of Pathology.
The authors report no conflict on interest.
Correspondence: Mehmet Harman, MD, Dicle Üniversitesi Tıp Fakültesi, Dermatoloji Anabilim Dalı, 21280 Diyarbakır, Turkey (mharman@dicle.edu.tr).

Scabies is a common ectoparasitic disease that can be diagnosed based on the presence of pruritus and typical clinical signs including burrows, vesicles, and erythematous papules. If a desquamative disease such as psoriasis precedes scabies, then the disease course may be altered. Pruritus may be absent and typical scabies lesions may be concealed due to the preexisting disease, resulting in delayed diagnosis. We present 2 cases of scabies in a brother and sister with erythrodermic psoriasis. In both cases peripheral hypereosinophilia suggested scabies. In patients with erythematous scaly inflammatory skin diseases who are treated with immunosuppressive agents, peripheral eosinophilia also could suggest scabies; therefore, a search for sarcoptic mites in skin scrapings should be undertaken.
Erythrodermic psoriasis is a severe form of psoriasis associated with higher morbidity and mortality rates compared to other forms of psoriasis. Cutaneous signs of erythrodermic psoriasis include erythema, edema, and superficial desquamation. Scabies is a common ectoparasitic disease that is diagnosed by the presence of pruritus and typical clinical signs including burrows, vesicles, and erythematous papules. Erythematous papules usually are distributed on the abdomen, thoracic region, axillae, and medial thighs and are characterized by more intense pruritus, especially at night. The course of scabies may be altered in patients with desquamative inflammatory skin disease such as psoriasis. Pruritus may be absent and typical scabies lesions may be concealed due to the preexisting disease, resulting in delayed diagnosis.
Case Reports
Patient 1
A 13-year-old adolescent boy with psoriasis of 4 years’ duration presented to our outpatient clinic with severe widespread erythema and mild desquamation (Figure 1). The patient was hospitalized following a diagnosis of erythrodermic psoriasis. His medical history was remarkable for recurrent episodes of bronchitis, and his family history included 2 siblings with psoriasis. Physical examination revealed no abnormalities, except for a fever (temperature, 38.0°C). A complete blood cell count revealed an elevated absolute eosinophil count (9260 cells/µL [reference range, 0–700 cells/µL]) corresponding to 48.4% (reference range, 0%–7%) of blood cells. There were no pathological findings in the serum biochemistry; complete urine analysis; throat, sputum, and urine cultures; stool analysis for parasites; or chest radiography. A VDRL test, hepatitis markers, and anti–human immunodeficiency virus test were negative. Antistreptolysin O titer; thyroid function tests; hormone profile; and IgG, IgA, IgM, C3, C4, and total IgE levels were within reference range. Peripheral blood smear, abdominal ultrasonography, electrocardiography, and echocardiography were performed; no cardiac pathology was observed. Cyclosporine 200 mg daily was initiated for treatment of erythrodermic psoriasis.
One week after the initiation of treatment the patient’s fever improved. At 2-week follow-up, a complete blood cell count demonstrated more marked eosinophilia, and the percentage of eosinophils at weekly intervals over the next 3 weeks increased to 51.2%, 63.0%, and 71.7%, respectively. The patient presented 2 weeks later with a chief concern of pruritus. Histologic examination of a lesional biopsy specimen revealed psoriasiform epithelial hyperplasia with scabies mites in the stratum corneum (Figure 2). Mites also were noted on direct microscopic examination of scrapings performed with the suspicion of scabies. The patient was treated with permethrin cream 5%. Although all of the patients and staff in the ward also were administered topical permethrin to prevent a scabies epidemic, 2 inpatients who had been discharged before the diagnosis of scabies presented to our outpatient clinic approximately 1 month later with scabies. At 6-month follow-up, the patient’s eosinophil count was within reference range (0.237cells/µL; 3.78%); pruritus and lesions were not observed.
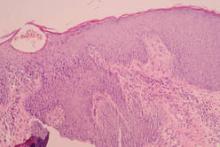 Figure 2. Findings from a lesional biopsy specimen demonstrated epidermal psoriasiform changes and eosinophils in the dermis. Mites were present in the stratum corneum (H&E, original magnification ×100). Figure 2. Findings from a lesional biopsy specimen demonstrated epidermal psoriasiform changes and eosinophils in the dermis. Mites were present in the stratum corneum (H&E, original magnification ×100).
Figure 2. Findings from a lesional biopsy specimen demonstrated epidermal psoriasiform changes and eosinophils in the dermis. Mites were present in the stratum corneum (H&E, original magnification ×100). Figure 2. Findings from a lesional biopsy specimen demonstrated epidermal psoriasiform changes and eosinophils in the dermis. Mites were present in the stratum corneum (H&E, original magnification ×100).
Figure 2. Findings from a lesional biopsy specimen demonstrated epidermal psoriasiform changes and eosinophils in the dermis. Mites were present in the stratum corneum (H&E, original magnification ×100).
Patient 2
A 26-year-old woman with psoriasis of 5 years’ duration was hospitalized for treatment of erythrodermic psoriasis at the same time as patient 1, her brother. On dermatologic examination, severe widespread erythema, scaling, and edema were noted (Figure 3). Physical examination revealed a fever (temperature, 38.5°C). Hypoalbuminemia and high C-reactive protein levels were present in serum biochemistry. Eosinophil counts were within reference range (0.346 cells/µL; 1.88%). No pathological findings were noted in the complete urine analysis; throat, sputum, and urine cultures; stool analysis for parasites; or chest radiography. A VDRL test, hepatitis markers, and anti–human immunodeficiency virus test were negative. Antistreptolysin O titer; thyroid function tests; hormone profile; and IgG, IgA, IgM, C3, C4, and total IgE levels were within reference range. Cyclosporine 200 mg daily was initiated for treatment of erythrodermic psoriasis. On days 20 and 45 of treatment, eosinophil levels were 8.26% (0.994 cells/mL) and 17.5% (1620 cells/mL), respectively. The patient’s erythema and edema remarkably decreased at the end of the first month of treatment with cyclosporine, but simultaneous onset of pruritus and increasing eosinophil levels despite treatment with cyclosporine were noted. Scabies mites were demonstrated on microscopic examination of skin scrapings from the dorsal aspect of the hand (Figure 4), and the patient was treated with permethrin cream 5%. At 6-month follow-up, eosinophil levels were within reference range (0.317 cells/mL; 4.75%); pruritus and lesions were not observed.
| Figure 3. Severe widespread erythema, scaling, and edema in a 26-year-old woman with psoriasis. |
Figure 4. A mite and an egg were noted on direct microscopic examination of skin scrapings from the dorsal aspect of the hand (original magnification ×400). |

Psoriasis and leprosy exist mutually exclusively with only a few cases being reported regarding their coexistence. Among the various forms of...
Psoriasis lesions typically are classified by their morphologic appearance and include plaque, guttate, pustular, and erythrodermic forms. Few...
Although rare, of all the cutaneous lymphoid malignancies, cutaneous T-cell lymphomas (CTCLs) constitute 65% of all lymphomas, of which 50% are...
