Article

Pemphigus Vulgaris in Pregnancy
We report the case of a 34-year-old woman who was diagnosed with pemphigus vulgaris (PV) during pregnancy. The patient presented with widespread...
Dr. Kahn is from the Department of Dermatology and Dermatologic Surgery, Medical University of South Carolina, Charleston. Dr. Friedmann was from the Division of Dermatology, Brody School of Medicine, East Carolina University, Greenville, North Carolina. Dr. Friedmann currently is from and Dr. Phillips is from Westlake Dermatology Clinical Research Center, Westlake Dermatology & Cosmetic Surgery, Austin, Texas.
The authors report no conflict of interest.
Correspondence: Daniel P. Friedmann, MD, Westlake Dermatology Clinical Research Center, Westlake Dermatology & Cosmetic Surgery, 8825 Bee Cave Rd, Ste 100, Austin, TX 78746 (daniel@westlakedermatology.com).

Although PV may have been considered a fatal disease at one time, treatment with systemic steroids has made it a manageable, albeit relapsing, condition. The development of corticosteroid-sparing, adjuvant immunosuppressives such as MMF has allowed for the more aggressive treatment of this disease with fewer steroid-related side effects.4,8,9 As seen in solid organ transplant recipients who often utilize combination therapy, the use of adjuvant immunosuppressives is associated with potential complications including bone marrow suppression and an increased risk for infections.7,10
Odynophagia is among the potential complications in patients with PV and has a wide differential diagnosis. Mucosal lesions of PV previously have been associated with HSV colonization, though a causal relationship has not been corroborated.5 Herpes simplex virus is more often detected in PV patients being treated with immunosuppressive agents than in nontreated patient groups.11 Recalcitrant or suddenly exacerbated oral mucosal lesions of PV under appropriate therapy may therefore be the result of HSV superinfection, which has been deferentially referred to as pemphigus herpeticum.12 Esophageal mucosal involvement by PV also may be more common than previously thought and should be suspected in patients with active oral disease.13 Esophagitis secondary to medications or various opportunistic organisms such as Candida, cytomegalovirus, or HSV also should be ruled out in patients taking immunosuppressives.5,10
Herpes esophagitis primarily occurs in immunocompromised hosts and is well documented in the literature regarding treatment with MMF and prednisone following renal and cardiac transplantation.10 Prednisone therapy in patients with chronic obstructive pulmonary disease also has been implicated.14 Reactivation of latent HSV resulting from immunosuppression is most often described, though primary infection also is possible.15 Patients typically present with acute odynophagia progressing to dysphagia, with complications ranging from sequelae of poor oral intake to esophageal perforation and hemorrhage, but the course generally is self-limited if immune function is promptly restored. Intravenous acyclovir has been known to hasten the recovery process and improve symptoms.16 Characteristic findings on esophagogastroduodenoscopy in combination with tissue biopsy, viral culture, and/or polymerase chain reaction aid in the diagnosis of herpes esophagitis.15,16 Our patient had a grossly abnormal esophagogastroduodenoscopy with positive cytology; however, no further diagnostic workup was performed. The cytologic findings and the rapid symptomatic improvement following the initiation of acyclovir helped support HSV as the etiology.
We present a case of herpes esophagitis that complicated the treatment of PV with MMF and prednisone. A diagnosis of herpes esophagitis must be ruled out in patients with PV who are undergoing therapeutic immunosuppression and present with an acute episode of odynophagia that is resistant to upscaling of therapy.

We report the case of a 34-year-old woman who was diagnosed with pemphigus vulgaris (PV) during pregnancy. The patient presented with widespread...
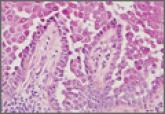
Hailey-Hailey disease typically presents as suprabasal blisters with a perivascular and interstitial lymphocytic infiltrate. The differential...

Dermatology residents often are on the front line when it comes to treating patients with complicated skin disorders, frequently seeing these...
