The accomplished gynecologic surgeon must know the anatomy of the retroperitoneal space in order to avoid damage to normal structures, as well as remove pathology. Many disease processes involve the pelvic peritoneum, uterosacral ligaments, rectosigmoid or ovarian pedicles, and require the surgeon to enter the retroperitoneal space to identify the ureters and blood vessels and keep them out of harm’s way. The challenges are complex:
- Badly distorted anatomy and the anterior and posterior cul-de-sac necessitate mobilization of the rectosigmoid and bladder.
- Intraligamentous fibroids require knowledge of the blood supply in the retroperitoneal space. Malignant disorders mandate that the lymph nodes be dissected to determine extent of disease and as part of treatment.
Is training adequate?
Every training program should teach the surgical anatomy of the retroperitoneal space, since every surgeon needs to be comfortable exposing the anatomy, both to prevent injury and to accomplish the needed surgery. Videotapes and cadaver courses can prepare the resident for the operating room.
The “landmark” umbilical ligament
The umbilical ligament was the umbilical artery in fetal life and courses along the edge of the bladder to the anterior abdominal wall up to the umbilicus. It is a useful guide into the perivesicle space. Lateral to it are the iliac vessels, and medial is the bladder. It is also a good marker for finding the right spot to open the round ligament.
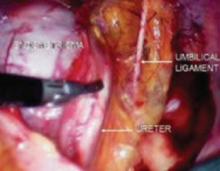
FIGURE 1 Opening the round ligament over the umbilical ligament
The round ligament is the key to exposing the retroperitoneal space. It should be open at the pelvic sidewall, just medial to the external iliac vessels. The umbilical ligament can be used as a landmark.
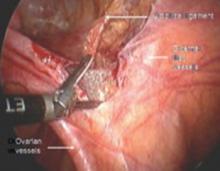
FIGURE 2 Opening lateral to the ovarian vessels
The divided round ligament is retracted ventrally and medially to place the ovarian vessels under traction. The peritoneum lateral to the ovarian vessels is divided up to the pelvic brim.
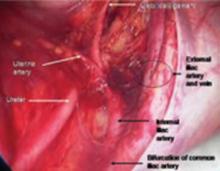
FIGURE 3 Right pelvic sidewall anatomy
Medial traction of the peritoneum around the ovarian vessels at the pelvic brim will expose the ureter coming over the iliac vessels at their bifurcation into external and internal branches.
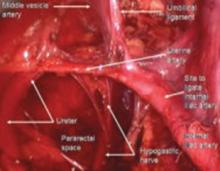
FIGURE 4 Relationship of ureter to the umbilical ligament
The ureter comes off medial with the fold of peritoneum. Once the space is developed, the operator’s finger or the laparoscopic probe can be introduced along the medial side of the internal iliac artery and ventral to the curve of the sacrum. This will open the pararectal space. The ureter and the anterior branch of the internal iliac artery are nearly parallel as they course through the pelvis.
FIGURE 5 Hypogastric nerve
The anterior branch of the internal iliac artery gives off the uterine artery and the middle and superior vesicle arteries before continuing on as the umbilical ligament.
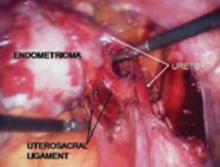
Endometriosis may imperil the ureter
Endometriomas and peritoneal implants are among the most common reasons for accessing the retroperitoneal space. Frequently the peritoneum between the ovarian vessels and the uterosacral ligaments (ovarian fossa) is thickened and retracted within the endometriosis implants. This alters the pelvic anatomy and puts the ureter at risk for injury.
Definitive surgical treatment for endometriosis includes removal of this diseased peritoneum. The ureter is best identified using the technique described, and then dissected off the peritoneum down to the uterine artery.
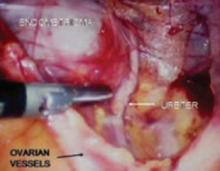
FIGURE 6 Finding the ureter lateral to an endometrioma
FIGURE 7 Relationship of ureter to the umbilical ligament
FIGURE 8 Dissecting the ureter out of the uterosacral ligament
The ureter may be placed on a Penrose drain to better isolate it and keep it under direct visualization. The cul-de-sac of Douglas is another site of endometrial implants. The fundus of the uterus is often adhesed to the rectosigmoid reflection and even the sigmoid colon. Nodules of endometriosis may infiltrate the uterosacral ligaments and extend into the rectovaginal space. To manage these implants, isolate the ureter to the point where it passes under the uterine artery.
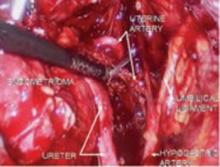
FIGURE 9 Divide uterine artery lateral to endometrioma
Here, the uterine artery is taken lateral to the mass, enabling the surgeon to remove all of the uterosacral implants. The bladder flap will be developed and the bladder advanced caudad. By dissecting medial to the ureter as it courses under the uterine artery, it will be retracted laterally and provide the space necessary to resect the uterosacral implants.
FIGURE 10 Rectosigmoid reflection with endometrioma nodule