From the Division of Allergy, Pulmonary, and Critical Care Medicine, Department of Medicine, Vanderbilt University Medical Center, Nashville, TN (Dr. Marra), Division of Anesthesiology Critical Care Medicine, Vanderbilt University Medical Center, Nashville, TN (Dr. Hayhurst, Dr. Hughes, Dr. Pandharipande), Department of Clinical and Experimental Science, University of Brescia, Brescia, Italy (Dr. Marengoni), School of Medicine and Surgery,
University of Milano-Bicocca, Milan, Italy (Dr. Bellelli), and Rehabilitation and Aged Care Unit Hospital Ancelle, Cremona, Italy (Dr. Morandi).
Abstract
- Objective: To present an overview of the phenomenon of inappropriate medication prescription in older critically ill patients and examine possible strategies of intervention.
- Methods: Review of the literature.
- Results: Polypharmacy and inappropriate prescribing of medications in older persons may lead to a significant risk of adverse drug-related events and mortality. The intensive care unit (ICU) is often the place where potentially inappropriate medications (PIMs) are first prescribed. Common PIMs at ICU discharge are antipsychotics, benzodiazepines, opioids, anticholinergic medications, antidepressants, and drugs causing orthostatic hypotension. Different classes of medications, typically intended for short-term use, are sometimes inappropriately continued after discharge from the hospital. At admission, potential risk factors for PIM are multiple morbidities, polypharmacy, frailty and cognitive decline; at discharge, a high number of pre-admission PIMs, discharge to a location other than home, discharge from a surgical service, longer length of ICU and hospital stay, and mechanical ventilation. Inappropriate prescribing in older patients can be detected through either the use of explicit criteria, drug utilization reviews, and multidisciplinary teams, including a geriatrician and/or the involvement of a clinical pharmacist.
- Conclusion: Use of PIMs may be common in critical patients, both on admission and at discharge from ICU. Therapeutic reconciliation is recommended at every transition of care (eg, at hospital or ICU admission and discharge) in order to improve appropriateness of prescription.
Key words: elderly; intensive care unit; inappropriate medications; antipsychotics.
Since older persons are often affected by multiple chronic diseases and are prescribed several medications, the quality and safety of prescribing these medications has become a global health care issue [1–4]. Polypharmacy and inappropriate prescribing of medications among the elderly is receiving significant attention in the medical literature [5,6]. Inappropriate medications in the elderly can lead to falls, cognitive impairment and delirium, poorer health status, and higher mortality [7–10]. Medications are considered potentially inappropriate when (a) the risks of treatment outweigh the benefits [11], (b) they are prescribed for periods longer than clinically indicated or without any clear indication, (c) they are not prescribed when indicated [12], and (d) they are likely to interact with other drugs and diseases. Medications included in this category are often referred to as potentially inappropriate medications (PIMs), as in some situations their use is justified; however, if the risk of harm from the drug is judged to outweigh the potential clinical benefit after an individual patient’s clinical circumstances are considered, these drugs are considered “actually inappropriate medications” (AIMs) [6].
Advancing age is associated with substantial pharmacokinetic and pharmacodynamics changes, such as altered distribution volumes and altered permeability of the blood-brain barrier, impaired liver metabolism and renal capacity, up- and down-regulation of target receptors, transmitters, and signaling pathways changes, impaired homeostasis, and increased risk of adverse drug reactions (ADRs) that lead to increased mortality and morbidity and higher health care costs [2,11,13–19]. Studies show that ADRs cause approximately 5% of hospital admissions in the general population, but the percentage rises to 10% in older persons [20].
Avoiding PIMs represents a strategy aimed at reducing drug-related mortality and morbidity. This article provides an overview of the phenomenon of inappropriate medication prescription in older critically ill patients and examines available strategies of intervention.
Inappropriate Medications at ICU Discharge
Though PIMs and AIMs may be identified at the time of hospital discharge, the intensive care unit (ICU) is often the place where these medications are first prescribed [21]. Acute hospitalization may increase PIM prescribing because of newly prescribed medications, the presence of multiple prescribers, inadequate medication reconciliation, and a lack of care coordination among inpatient providers or in the transition back to outpatient care [22)].
A known complication of critical illness and ICU stay is a significant increase in psychological symptoms, sleep cycle alterations, delirium, and cognitive impairment, which may be associated with increased prescription of specific PIMs, such as antipsychotics or benzodiazepines [6,23,24]. Despite the lack of reliable evidence supporting their use in the ICU, antipsychotic agents are used routinely in ICU patients [25] to treat a variety of conditions, such as substance withdrawal, agitation not responding to other therapies, or delirium. Results from a multicenter study of 164,996 hospitalizations across 71 academic medical centers in the US showed that 1 out of 10 ICU patients received an antipsychotic during their hospital stay [25]. Jasiak et al estimated that one-third of patients initiated on an atypical antipsychotic therapy for ICU delirium received a hospital discharge prescription for these medications, with a potential annual outpatient medication cost of approximately $2255 per patient [26].
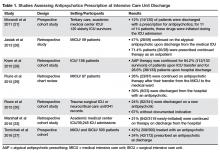
One potential consequence of antipsychotic use in the ICU is their continuation after the transition to other clinical settings, including discharge from the hospital [27] (Table 1).
A study of 120 elderly ICU survivors found that 12% (14/120) of patients were discharged with a prescription for antipsychotics and for 11 of 14 patients, these drugs were initiated during the ICU admission [21]. Another single-center retrospective study of 59 medical ICU patients showed that antipsychotics were continued in 47% of patients at ICU discharge and in 32% of patients at hospital discharge [26]. Kram et al conducted a retrospective cohort study of 156 patients admitted to an ICU who received at least two doses of an antipsychotic for delirium [28]. Of the 133 survivors, antipsychotic therapy was continued for 84.2% patients upon ICU transfer and for 28.6% patients upon hospital discharge, despite the majority of these patients having evidence of delirium resolution or no indication for continuation of these medications [28]. Similar results were shown by Flurie et al, who found that 26% of patients (23/87) were continued on antipsychotic therapy after their discharge from the medical ICU to the medical ward. Of the 23 patients continued on antipsychotic therapy, 39% (9/23) were discharged from the hospital with an antipsychotic [29]. In a recent study, Tomichek et al showed that 1 out of every 4 antipsychotic-treated patients was discharged on an antipsychotic even though the majority was no longer delirious [27].When examining the specific factors that may contribute to a patient being discharged on an antipsychotic, authors found that the specific antipsychotic used correlated with risk of continuation [27,30], with atypical antipsychotics having a greater likelihood of being continued than haloperidol [27,30]. Possible explanation for these results could be that physicians perceive less long-term risk from atypical agents, so may be more likely to continue them on discharge [30]. However, such an approach is not always safe. Indeed, although atypical antipsychotic agents tend to cause less tardive dyskinesia, they are known to be associated with similar rates of other adverse events compared with typical agents and have been linked to an increased risk of sudden cardiac death and pneumonia in the elderly [31,32].
Other factors independently associated with being discharged on a new antipsychotic medication were the severity of the acute illness as measured with the Acute Physiology and Chronic Health Evaluation II score at ICU admission (odds ratio [OR] 1 [95% confidence interval {CI}, 1.0–1.1]) and days treated with benzodiazepines (OR 1.1 [95% CI, 1.0–1.14]) [30]. Conversely, perhaps due to different practice patterns, Tomichek et al did not find an association between benzodiazepines administration and antipsychotic prescription at discharge in post hoc analyses [27].
Another possible reason for antipsychotic continuation may reside in the indication chosen [33]. Antipsychotic agents have sedative properties and they might be used to optimize sleep during hospitalization, despite the lack of evidence to support this indication [34]. Other factors potentially contributing to continuation of antipsychotics may include persistent delirium and agitation, newly diagnosed psychiatric illness, and difficulties experienced by physicians in deprescribing [35] with improper/incomplete medication reconciliation [33].
The continuation of antipsychotic therapy increased 30-day readmission rates in patients compared to those who had therapy stopped before discharge [33]. In addition to the well-described cardiac effects (prolonged QT interval), neuroleptic malignant syndrome and extrapyramidal symptoms may also occur, and longer-term use can predispose patients to metabolic disturbances, falls, and increase the risk of death in elderly patients with dementia [31].
Benzodiazepines and sedative hypnotics are commonly used to treat insomnia and agitation in older adults despite significant risk. Benzodiazepine administration was found to be an independent risk factor for a daily transition to delirium [36,37]. Pandharipande et al reported that every unit dose of lorazepam was associated with a higher risk for daily transition to delirium (OR 1.2, 95% CI 1.1–1.4, P = 0.003) [36] in critically ill patients. A more recent analysis found for every 5 mg of midazolam administered to a patient who is awake and without delirium, there is a 4% chance that this patient will develop delirium the next ICU day [37].
Given that the risk for benzodiazepine-associated delirium is dose-dependent, clinicians should use strategies known to reduce the daily number of benzodiazepines administered that often includes the use of a sedative associated with less delirium occurrence, such as dexmedetomidine or propofol [38]. Evidence has shown that long-term use of benzodiazepines has little benefit with many risks, including an increased susceptibility to spontaneous bacterial infection [39,40] and mortality in the setting of infection [41]. Nakafero et al showed that exposure to benzodiazepines was associated with increased occurrence of both influenza-like-illness–related pneumonia and mortality. Benzodiazepine use was associated also with increased occurrence of asthma exacerbation and with increased all-cause mortality during a median follow-up of 2 years in a cohort of asthmatic patients [42] as well with an increased risk of pneumonia and long-term mortality in patients with a prior diagnosis of community- acquired pneumonia [40]. Long-term use of benzodiazepines is also associated with increased risk of falls [43–45], cognitive impairment [46–48] and disability [49,50].
Other common types of PIMs at ICU discharge were opioids, anticholinergic medications, antidepressants, and drugs causing orthostatic hypotension [6]. Of the anticholinergic AIMs, H2 blockers (61%) and promethazine (15%) were the most common [6]. Only 16% of opioids, 23% of antidepressants, and 10% of drugs causing orthostatic hypotension were found to be actually inappropriate after the patient’s circumstances were considered (eg, postoperative pain control, a new diagnosis of major depressive disorder) [6].