DISCUSSION
According to the Juvenile Diabetes Research Foundation, as many as 1.25 million Americans are currently living with T1D; from 2001 to 2009, the prevalence of T1D in people younger than 20 increased by 23%.1 The overall prevalence of diabetes (both types 1 and 2) is predicted to be one in every three people by 2050 if current trends continue.2 According to the American Diabetes Association (ADA), 18,436 US youths are diagnosed with T1D every year, and T1D accounts for about 5% of diabetes cases in the US population.2
Diagnosis
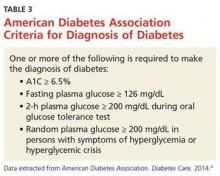
Diabetes is diagnosed based on blood test results that fall within the parameters set by the ADA diagnostic criteria (see Table 3).3 In addition to diagnostic testing for diabetes recommended by the ADA guidelines, blood tests are ordered for autoantibodies that are associated with T1D, to distinguish between type 1 and type 2 diabetes. (T1D results from cellular-mediated autoimmune destruction of the insulin-producing beta cells in the pancreas.4) Upon initial diagnosis, about 85% to 90% of T1D patients have one or more autoantibodies present in blood work, such as autoantibodies to islet cells or to insulin, glutamic acid decarboxylase (GAD65), or tyrosine phosphatases IA-2 and IA-2B.4
In this case study, the child had an elevated GAD65 value and a positive screening for an insulin autoantibody, which explained the destruction of her beta cells. The patient also had KP and xerosis, which are clinical manifestations commonly seen in T1D. In one study of children with T1D, 22% had xerosis, compared with 3% of healthy, age-matched controls, and KP was also significantly more common in T1D patients than in controls (12% vs 1.5%).5
The presence of ketones in the case patient’s urine also suggests T1D, rather than type 2.4 The differential diagnosis for T1D includes type 2 diabetes mellitus, monogenic diabetes mellitus (formerly known as maturity-onset diabetes of the young), secondary hyperglycemia, and other endocrine disorders.6
Acute complications associated with T1D include hypoglycemia, hyperglycemia, and DKA. Long-term complications may include diabetic retinopathy, cataracts, gastroparesis, hypertension, renal failure, coronary artery disease, peripheral vascular disease, diabetic neuropathy, and increased risk for infection.7 These complications can likely be prevented by good glycemic control, proper diet, exercise, and avoidance of nicotine.7
Unfortunately, T1D cannot currently be prevented, although research studies are under way. TrialNet is currently conducting a “Pathway to Prevention” trial; the researchers are testing ways to delay and prevent T1D, as well as slow its progression after diagnosis.8 Potential participants (family members of a T1D patient) are screened for T1D autoantibodies. If test results are positive, these participants are included in the prevention pathway study.
Continue for management >>