Meniscectomy is the most common orthopedic procedure performed in the United States with 700,000 meniscectomies performed every year.1 More than half of these procedures are performed in patients ≥45 years of age,2 giving rise to the question: Does arthroscopic surgery have a role in the treatment of patients who may have osteoarthritis (OA) and another knee condition, such as a symptomatic meniscal tear? Determining the answer is especially important when you consider that the number of true and incidental tears diagnosed on magnetic resonance imaging (MRI) has been on the rise3—a result of the routine use of MRIs to identify the cause of patients’ chronic knee pain.
At a cost of roughly $5,000 per procedure, some experts have suggested that at least a portion of the approximately $4 billion annual direct medical costs associated with meniscectomy could be put to better use.4,5 This prompted us to wonder what the literature tells us about the management of degenerative meniscus tears in middle-aged patients with OA and whether these patients would benefit from nonoperative management with optimized physical and medical therapy as a first-line approach. Our findings follow.
But first, a word about the connection between OA and meniscal tears.
What we’ve learned about meniscal damage
Research has shown that over one-third of individuals >50 years of age and three-quarters of people with knee OA have degenerative meniscal tears.6 In the past, the relative paucity of epidemiologic data on the prevalence of meniscal tears in the general population made it difficult to interpret the diagnostic information provided by MRI.
More recently, experts found that meniscal damage is especially prevalent among individuals with OA, and they began treating with arthroscopic partial meniscectomy (APM), as the meniscal damage was thought to be the anatomical foundation for the complaint of knee pain.7
However, researchers then began realizing that many patients with findings of a meniscal tear visualized on MRI reported no knee symptoms. In one study, adults in a large community-based sample found to have a meniscal tear on MRI were no more likely to have knee pain than subjects without a meniscal tear.6 Similarly, subjects with a meniscal tear and OA had no more severe pain than subjects with OA and no meniscal tear.6
In addition, the landmark Fairbank study from 19488 and others since have shown that meniscectomy can lead to other problems. Removal of meniscal tissue decreases the contact stress area, which increases stress on the articular cartilage, and inevitably leads to degeneration of the involved joint.9 Researchers have shown that even partial meniscectomy produces late articular cartilage changes.10
Which interventions and when?
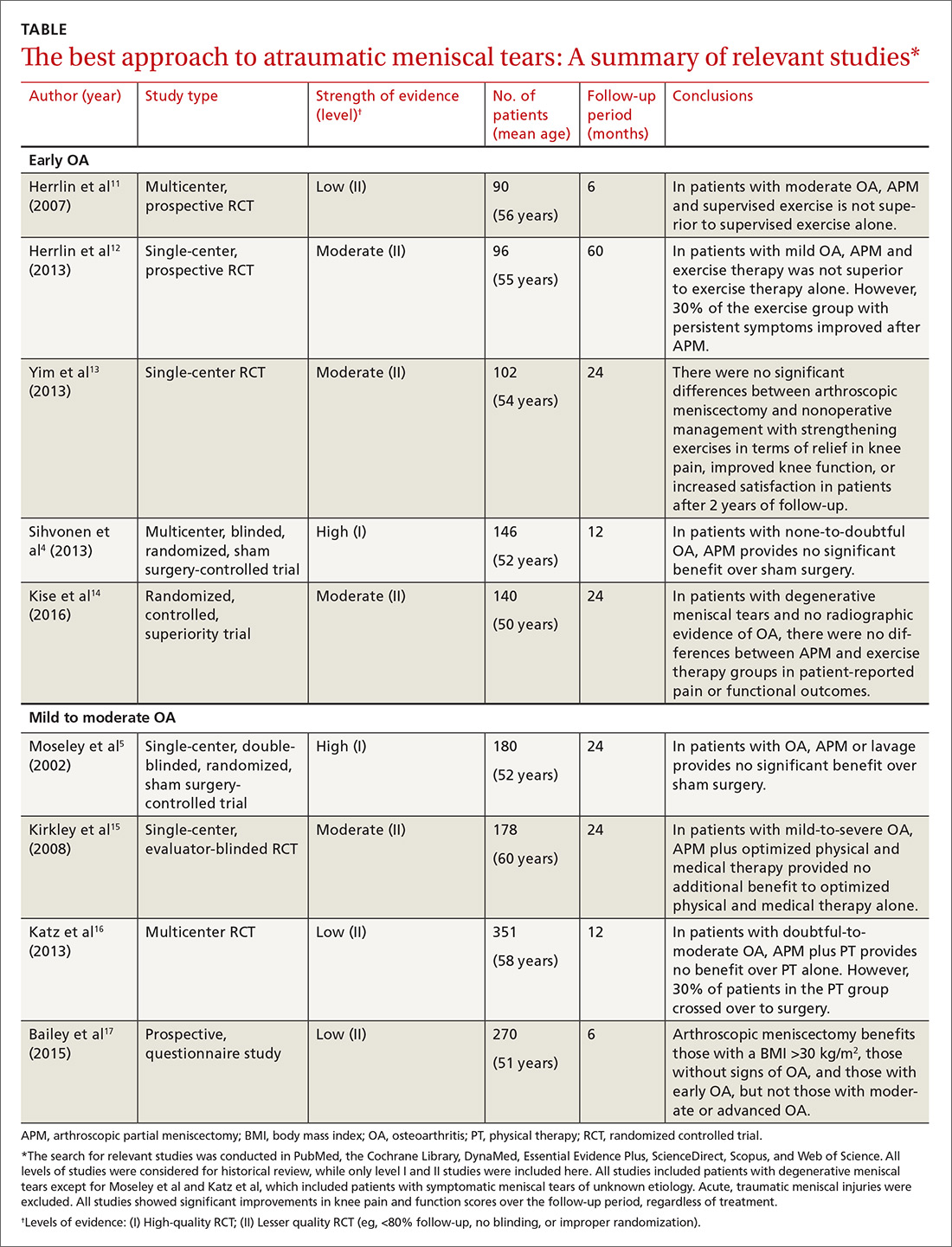
We conducted an in-depth literature review to determine which approaches were best for the treatment of OA and meniscal tears, and summarize our findings below, according to OA severity. (For details of how the literature review was conducted and an at-a-glance summary of the key findings, see the TABLE.4,5,11-17) Of note: All of the studies reviewed here included patients with chronic knee pain and excluded patients with sudden onset pain from a single physical event.
The findings: Early OA and meniscal tears
The first 2 studies we identified in the literature, both published by Herrlin et al,11,12 examined the efficacy of APM in middle-aged patients with early OA (≤grade 1), according to the Ahlbäck classification.
In the first Herrlin study, a 6-month prospective randomized trial, 90 middle-aged patients with a medial meniscal tear (without traumatic history) were assigned to either APM followed by supervised exercise or 8 weeks of supervised exercise alone.11 Exercise consisted of activities for improving muscle strength, endurance, and flexibility, as well as for balance and proprioception. The authors concluded that a combination of APM and supervised exercise did not lead to greater improvements in knee function compared with supervised exercise alone.11
In the second Herrlin study, a prospective randomized study involving 96 middle-aged patients with an MRI-verified medial meniscal tear and radiographic OA, the authors concluded that arthroscopic surgery followed by exercise therapy was not superior to the same exercise therapy alone.12 The results were gleaned from both patient-reported outcomes and radiographic assessment at 2 and 5 years. Both groups reported significant improvements at 5 years, but participants did not reach the level of fitness and quality of life of similarly-aged healthy controls.
Perhaps one of the most interesting aspects of this study was that approximately one-third of patients from the exercise-only group still had disabling knee symptoms after exercise therapy, but improved to the same level as the rest of the patients after crossing over and undergoing APM.12 Part of the observed benefit of arthroscopy in these patients has the potential to be explained by the placebo effect, especially given that invasive procedures have a stronger placebo effect than do noninvasive ones, and due to the lack of blinding.18 Additionally, limitations of the above studies include small sample sizes, lack of a control group, and short-term follow-up.
Next, a 2013 study by Yim et al looked specifically at APM vs nonoperative treatment with strengthening exercises.13 A total of 102 patients with an average age of 53.8 years, a Kellgren-Lawrence Classification of Osteoarthritis of <2, and an MRI-confirmed degenerative horizontal tear of the posterior horn of the medial meniscus were randomized to the 2 intervention groups. The 2 groups were highly comparable, giving the study high internal validity. These patients were then assessed at 3 months, one year, and at 2 years after treatment.
Although most patients at the outset of the study had intense knee pain with mechanical symptoms, both groups reported a decrease in experienced knee pain, improved function, and a high level of satisfaction with their prescribed treatment, with no significant difference in any of these values after 2 years of follow-up.13 A limitation of the study was that it used subjective questionnaires to assess pain, swelling, and activities of daily living (ADLs).
A fourth study, a 2013 multicenter, randomized, sham-controlled trial, looked at 146 patients ages 35 to 65 years who had knee symptoms consistent with a degenerative medial meniscus tear (confirmed by MRI and arthroscopic evaluation) and no knee arthritis.4 The subjects were assigned to either APM or sham surgery (skin incisions only). The results showed that APM was not superior to sham surgery with regard to outcomes assessed during a 12-month follow-up period.4
Most recently (2016), Kise et al14 published the results of a randomized controlled superiority trial conducted in Norway comparing 12 weeks of supervised exercise therapy with APM for patients with degenerative meniscus tears. Their study included 140 patients ages 36 to 60 years. Notably, most (96%), but not all, of their patients had no radiographic evidence of OA.
At the 2-year follow-up, there were no differences in patient-reported pain or functional outcomes, with all patients improving significantly from baseline. Muscle strength was also measured and found to be significantly greater at 3 and 12 months in the exercise group. Limitations of this study were a lack of patient blinding and a 19% crossover from the exercise to the APM group.