After a night of heavy drinking, a 34-year-old man awakens with a rapid heart rate and a fluttering sensation in his chest, which radiates up to his neck. By the time he arrives to your emergency department, he has had these symptoms for about 2 hours. He denies chest pain but reports having difficulty catching his breath. He says this is the first time he’s experienced these symptoms. He has no prior cardiac or pulmonary history.
The patient had been out with 4 old college friends, and they had between them consumed a case of beer and a fifth of whiskey. He cannot remember going home, but they all had ordered cabs ahead of time, knowing they would be drinking heavily. He denies taking any recreational drugs.
Past medical and surgical histories are remarkable only for a left tibial fracture sustained when the patient played high school football. He has no allergies and takes no medications. Although he doesn’t smoke tobacco, he admits to using marijuana sparingly; however, he says he hasn’t used it in the past 3 months. He works as a store manager at a local grocery chain. He isn’t married, has no children, and isn’t in a relationship.
Family history reveals the patient is an only child. His father has hypothyroidism, and his mother has type 2 diabetes, which is controlled with metformin. His maternal grandparents both have hypertension, which is managed with β-blockers. His paternal grandparents are both deceased as a result of an automobile accident, and he does not know whether they had any significant medical illnesses.
The review of systems shows a recent increase in alcohol consumption following a breakup with his girlfriend 3 months ago. A 12-point review of systems is noncontributory.
Vital signs include a blood pressure of 118/62 mm Hg; pulse, 150 beats/min; and O2 saturation, 98% on room air. He is afebrile.
Physical exam reveals a thin, healthy but anxious man. His height is 72 in and his weight, 188 lb. The HEENT exam is normal. The neck is supple without thyromegaly and no jugular venous distention. The lungs are clear in all fields without wheezes, rales, or rhonchi.
Cardiac exam reveals tachycardia with a regular rate of 150 beats/min and no murmurs, extra heart sounds, or rubs. The abdomen is soft and nontender, with no palpable organomegaly. Peripheral pulses are equal bilaterally, with no palpable bruits. There is no peripheral edema, and the neurologic exam is intact.
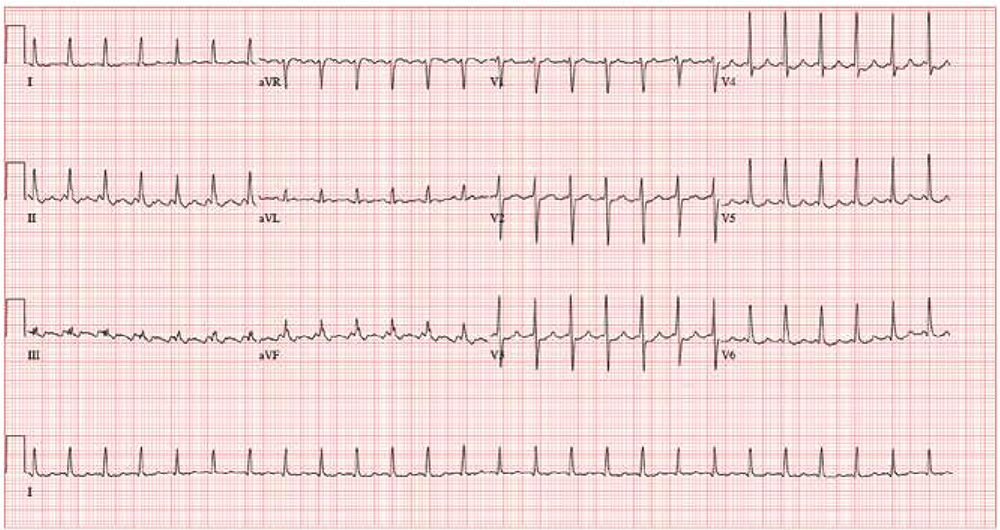
An ECG reveals the following: a ventricular rate of 155 beats/min; PR interval, unmeasured, QRS duration, 78 ms; QT/QTc interval, 272/437 ms; P axis, unmeasured; R axis, +34°; and T axis, –50°. What is your interpretation?