Ms. M, a generally healthy 55-year-old woman, was diagnosed recently with severe vitamin D deficiency (serum 25-hydroxyvitamin D [25(OH)D] level of 8 ng/mL). She presents with her second episode of acute viral bronchitis in the past 6 months. She has no history of significant smoking or exposure or history of asthma and does not take respiratory medications. Standard treatment for her level of vitamin D deficiency is 50,000 IU/wk in bolus dosing—but is that your best option for the patient?
ARTIs include nonspecific upper respiratory illnesses, otitis media, sinusitis (~70% viral), pharyngitis, acute bronchitis (also ~70% viral), influenza, respiratory syncytial virus, and pneumonia.1,2 In the United States, ARTIs strain the health care system and are the most common reason for ambulatory care visits, accounting for almost 120 million (about 10% of all) visits per year.3 In addition, ARTIs account for almost 50% of antibiotic prescriptions for adults and almost 75% of antibiotic prescriptions for children—many of which are unnecessary.2,4
While patient and parent education, antibiotic stewardship programs, and demand management may reduce inappropriate antibiotic use and the overall burden of ARTIs on the health care system, prevention of infections is a powerful tool within the overall approach to managing ARTIs.
STUDY SUMMARY
Vitamin D is protective in smaller doses
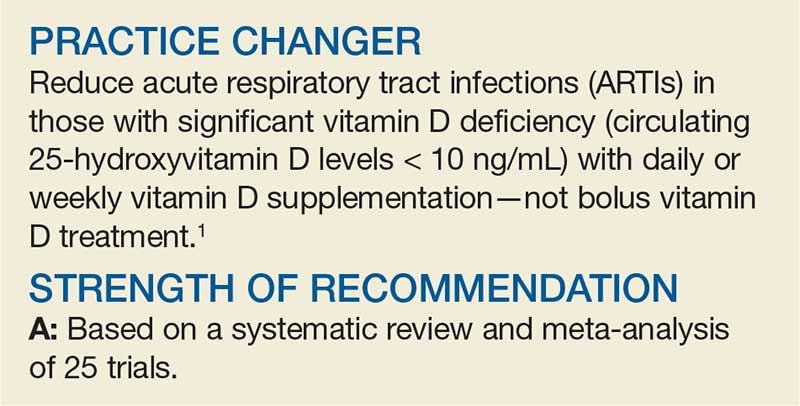
This 2017 systematic review and meta-analysis of 25 trials (N = 10,933) evaluated vitamin D supplementation for the prevention of ARTIs in the primary care setting. Individual participant data were reevaluated to reduce risk for bias. The Cochrane risk-for-bias tool was used to address threats to validity.
The study included institutional review board–approved, randomized, double-blind, placebo-controlled trials of vitamin D3 or D2 supplementation of any duration and in any language. The incidence of ARTI was a prespecified efficacy outcome. Duration of the included randomized controlled trials (RCTs) ranged from 7 weeks to 1.5 years.
Outcomes. The primary outcome was an incidence of at least 1 ARTI. Secondary outcomes included incidence of upper and lower ARTIs; incidence of adverse reactions to vitamin D; incidence of emergency department visits or hospital admission or both for ARTI; use of antimicrobials for ARTI; absence from work or school due to ARTI; and mortality (ARTI-related and all-cause).
Findings. Daily or weekly vitamin D supplementation (in doses ranging from < 20 to ≥ 50 µg/d) reduced the risk for ARTI (adjusted odds ratio [AOR], 0.88; number needed to treat [NNT], 33). In subgroup analysis, daily or weekly vitamin D was protective (AOR, 0.81), but bolus dosing (≥ 30,000 IU) was not (AOR, 0.97).
In 2-step analysis, patients benefited if they had baseline circulating 25(OH)D concentrations < 10 ng/mL (AOR, 0.30; NNT, 4); had baseline circulating 25(OH)D levels of 10 to 28 ng/mL (AOR, 0.75; NNT, 15); were ages 1.1 to 15.9 (AOR, 0.59); were ages 16 to 65 (AOR, 0.79); or had a BMI < 25 (AOR, 0.82).
Higher D levels are a different story. Vitamin D supplementation in people with circulating levels of 25(OH)D ≥ 30 ng/mL did not appear to provide benefit (AOR, 0.96). Supplementation in this population did not influence any of the secondary outcomes, including risk for all-cause serious adverse events (AOR, 0.98).