ANSWER
The correct answer is argyria (choice “d”), caused by the ingestion of colloidal silver. Wilson’s disease (choice “a”) is an inherited disorder of copper metabolism involving signs of liver failure, including jaundice. Addison’s disease (choice “b”), also known as hypoadrenalism, can present with generalized hyperpigmentation, but also with symptoms such as extreme fatigue and hypotension—both of which are missing in this case. Hemochromatosis (choice “c”) is a defect in iron storage that can, among other things, involve hyperpigmentation of the entire body, but not with bluish discoloration.
DISCUSSION
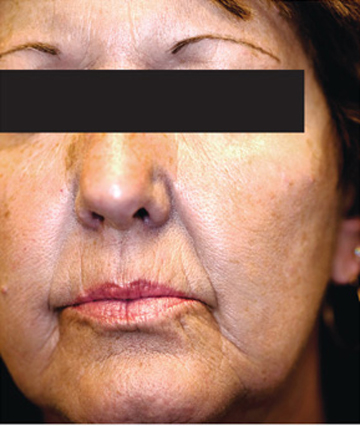
Ingestion of silver or its salts has long been associated with slate gray to bluish discoloration of skin, mucosal surfaces, and internal organs (including the nervous system), a condition termed argyria. In skin, silver is mostly deposited around adnexal structures in the dermis, producing discoloration thought to result from the presence of silver and silver-induced increase in melanin concentration. The effect is most pronounced in sun-exposed skin.
The degree, extent, and duration of this discoloration depends in part on the total intake of silver. Unlike most other causes of hyperpigmentation (eg, from minocycline or hemochromatosis), argyria tends to be permanent.
Aside from the above-mentioned differential items, other possible lookalikes include methemoglobin, polycythemia, and carcinoid syndrome. Additionally, a number of drugs (eg, antimalarials, chlorpromazine, minocycline, amiodarone) or other metals (eg, gold, bismuth) can produce similar effects.
In the past few years, with the increased interest in alternative medicine—in part bolstered by the availability of information and even product over the Internet—the use of colloidal silver products has been on the rise again. These products were extremely popular into the early twentieth century, but by 1999, the FDA had ruled that the risks of silver-containing products exceeded any currently understood benefits. The agency banned the use of silver in any OTC products, but that ruling did not apply to its use in dietary products. So colloidal silver–containing products are once again being touted for all manner of maladies such as AIDS, cancer, arthritis, and infectious disease. There have been reports of ingestion of large amounts of silver salts causing hemolysis, pleural edema, or even coma.
Topically applied silver-containing products are known in some cases to have antibacterial effects. For example, silver sulfadiazine 1% cream has been used to treat burns since 1967, although the application of silver to skin to prevent or treat infection was first described centuries ago.
As for our patient, her new coloration will likely be permanent, since no effective treatment exists.