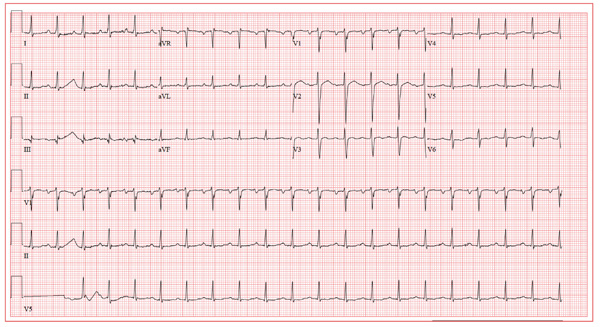
A 39-year-old business professional returns to your clinic for follow-up one month after a synchronized cardioversion to treat abrupt-onset atrial flutter (see January 2012 ECG Challenge). He is slightly short of breath, he says, because he ran up six flights of stairs to see you in clinic after undergoing an echocardiogram. Briefly, he developed atrial flutter presumably as a result of consuming a large quantity of caffeinated coffee along with several energy drinks containing taurine. He has been under a significant amount of stress at work for the past six months, working on a project that he predicted would play a major role in his career. The deadline has come and gone, and his business transaction was a success. He has taken your advice to avoid energy drinks, consume coffee in moderation, stop smoking, get plenty of rest, and exercise. His affect is much improved. He is pleasant, jovial, and relieved that he has had no subsequent episodes of atrial flutter. His medical history is remarkable for that single episode of atrial flutter, as well as childhood cases of chickenpox and mumps. He is taking ibuprofen for a sore knee as a result of “too much basketball.” He has no known drug allergies. Following his cardioversion, his alcohol consumption decreased from two cocktails in the evening and a 12-pack of beer on the weekends to an occasional cocktail during the week and two to four beers on the weekends. He denies illicit drug use. The review of systems is unremarkable. The physical exam reveals a thin, well-developed man in no distress. His weight is 170 lb and his height, 74”. Vital statistics include a blood pressure of 128/72 mm Hg; pulse, 110 beats/min; respiratory rate, 16 breaths/min; temperature, 98.4°F; and O2 saturation, 100% on room air. The chest is clear to auscultation in all lung fields. There are no murmurs, rubs, clicks, or extra heart sounds. The abdomen is soft and nontender. The pulses are equal and bounding bilaterally. The neurologic exam is benign. The echocardiogram performed earlier shows a left ventricular ejection fraction of 68%, normal left and right ventricular volumes and function, normal valvular function, and a left atrial measurement of 3.8 cm (normal, 1.6 to 4.0 cm). An ECG performed just before you entered the exam room reveals the following: a ventricular rate of 122 beats/min; PR interval, 184 ms; QRS duration, 90 ms; QT/QTc interval, 282/401 ms; P axis, 24°; R axis, 28°; and T axis, –45°. What is your interpretation of this ECG?