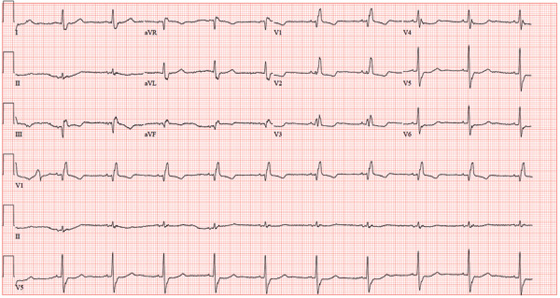
An 84-year-old woman presents with left-sided chest pain radiating to the back and neck. The pain began about four hours ago, while she was knitting. She describes it as a “dull ache” that quickly progressed to a “sharp, sticking” pain on a scale of 8/10. She has never experienced pain like this before. She denies nausea, vomiting, diaphoresis, headache, palpitations, orthopnea, or dyspnea on exertion. Her medical history is remarkable for Crohn’s disease, atrial fibrillation, hypertension, and myxomatous mitral valve disease. Surgical history is remarkable for a myocardial infarction 10 years ago, two separate catheter ablations for atrial fibrillation (successful on the second attempt), a mitral valve replacement (bioprosthetic) one year ago, and a hysterectomy/oophorectomy in the remote past. The patient has no known drug allergies. Her medications include atenolol, aspirin, furosemide, estradiol, ferrous sulfate, mesalamine, omeprazole, warfarin, and lisinopril. She is a retired teacher, married, who has never smoked and rarely drinks alcohol. Her family history is remarkable for heart disease in her father and diabetes in her mother. The review of systems is negative, with the exception of frequent episodes of nonbloody diarrhea and abdominal pain associated with her Crohn’s disease. Physical exam reveals a blood pressure of 208/120 mm Hg; pulse, 60 beats/min; respiratory rate, 22 breaths/min-1; temperature, 97.8°F; and O2 saturation, 96% on 2L oxygen. She appears anxious, restless, and unable to find a comfortable position. Pertinent physical findings include jugular venous distention to the angle of the jaw, a regular heart rate with a harsh III/VI systolic murmur at the left upper sternal border, and a soft II/VI diastolic murmur radiating to the apex. Peripheral pulses are brisk and equal bilaterally. There are no neurologic deficits. Laboratory data include a normal complete blood count, an INR of 2.2, normal blood chemistries, normal liver function studies, and negative troponin levels. CT reveals a 5.5-cm dissection of the ascending aorta. An ECG shows the following: a ventricular rate of 61 beats/min; PR interval, 108 ms; QRS duration, 132 ms; QT/QTc interval, 478/481 ms; P axis, 19°; R axis, 0°; and T axis, –13°. What is your interpretation of this ECG?