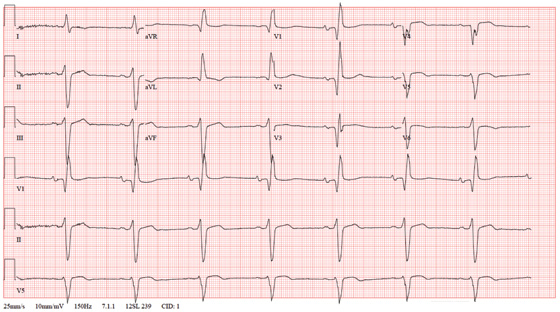
A 72-year-old man presents for a routine appointment. He was doing well until two months ago, when he started to notice that he fatigues easily. He is unable to go up and down stairs at home without pausing and has difficulty working in his garden. He says he does not become short of breath but just feels fatigued. The patient denies chest pain, palpitations, tachycardia, syncope, or near-syncope. He denies recent weight gain or peripheral extremity edema. He has had no recent changes to his medications, and he has not recently been ill. The man’s cardiac history is remarkable for coronary artery disease, a coronary artery bypass graft (CABG) in 2007, paroxysmal atrial fibrillation, and an ischemic cardiomyopathy. His most recent echocardiogram (six months ago) showed global left ventricular dysfunction with inferior akinesis, a left ventricular end-diastolic dimension of 8.1 cm, and a left ventricular ejection fraction of 35%. His pulmonary artery pressure was 25 to 29 mm Hg. A nuclear viability study performed at the same time showed a nonviable myocardial infarction involving the anterior and inferior septal walls of the left ventricle. A cardiac catheterization performed one year ago showed 30% stenosis of the left main coronary artery, an occluded left anterior descending (LAD) artery with myocardial perfusion supplied by right-to-left collateral vessels, 50% stenosis of the left circumflex artery, 70% stenosis of the left circumflex artery, and 70% to 80% stenosis of the mid right coronary artery (RCA). The saphenous vein grafts to the LAD, RCA, circumflex, and diagonal branches were occluded. Medical history is remarkable for dyslipidemia, arthritis, and depression. In addition to CABG, surgical history includes cholecystectomy and a left hip replacement. The patient is a retired beer distributor who has lived alone since his wife’s death three years ago. He drinks two or three glasses of wine in the evenings. Prior to quitting 10 years ago, he had a 30-pack-year history of smoking; however, he started again after his wife’s death and currently smokes half a pack of cigarettes per day. His medication list includes aspirin, atenolol, hydrochlorothiazide, lisinopril, atorvastatin, and trazodone. The review of systems is negative. Vital statistics include a blood pressure of 106/58 mm Hg; pulse, 50 beats/min; temperature, 97.5°F; and O2 saturation, 94% on room air. His weight is 172.4 lb and is unchanged from his last clinic visit. Pertinent findings on the physical exam include clear lung fields, a regular rhythm, and bradycardia with no murmurs or extra heart sounds, no bruits, no jugular venous distention, and no peripheral edema. All pulses are equal and normal. Based on the patient’s symptoms and the finding of bradycardia on physical exam, you order an ECG, which shows the following: a ventricular rate of 46 beats/min; PR interval, 202 ms; QRS duration, 200 ms; QT/QTc interval, 578/505 ms; P axis, 71°; R axis, –77°; and T axis, 109°. What is your interpretation of this ECG?