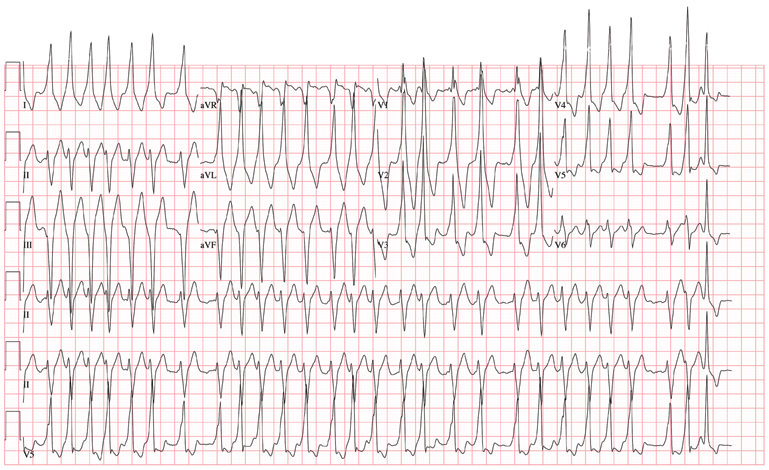
The charge nurse in the emergency department (ED) calls to tell you that one of your patients, a 19-year-old man, has just presented with a three-hour history of continuous palpitations. She reports the patient’s pulse as 170 beats/min and adds that although he is awake and stable, he is complaining of chest discomfort and lightheadedness. The tachycardia began abruptly while the patient was playing basketball. Witnesses said he did not lose consciousness but did sit down, complaining of dizziness. The patient admits he thought he “was going to pass out” when he sat up. As you review the patient’s chart, you recall seeing him for palpitations approximately six months ago, at which time an ECG showed Wolf-Parkinson-White (WPW) syndrome with a left-sided accessory pathway. His history is remarkable for palpitations beginning at age 14, with two episodes of near-syncope. None of his episodes of palpitations has lasted as long as the current one, however. Medical history is remarkable for a tonsillectomy at age 7. Family history is positive for coronary artery disease and diabetes. The patient takes no medications and has no known drug allergies. He is a college student, drinks a six-pack of beer on weekends despite being under age, and tried marijuana once. He denies any other use of illegal, illicit, or performance-enhancing drugs. The review of systems is noncontributory. The physical exam reveals a thin, anxious male. His blood pressure is 98/66 mm Hg; pulse, 170 beats/min; respiratory rate, 16 breaths/min; temperature, 99°F; and O2 saturation, 98% on 2L of oxygen. There is no jugular venous distention, and carotid upstrokes are rapid and brisk. The chest is clear to auscultation bilaterally with good excursion. The cardiac exam reveals a rapid, regular rate with no murmurs, gallops, or rubs. There are no extra heart sounds. The abdominal, peripheral, and neurologic exams are intact without focal signs. On arrival in the ED, you are handed an ECG, which shows: a ventricular rate of 174 beats/min; PR interval, not measured; QRS duration, 164 ms; QT/QTc interval, 302/513 ms; no P axis; R axis, –46°; and T axis, 118°. What is your interpretation of this ECG?