Kidney or urinary tract stones (whose presence is referred to as nephrolithiasis) are hard, crystalline mineral concretions that form within the kidney or the urinary tract. They are a common problem, with an estimated annual incidence of 1% and a lifetime risk of 15% to 25%; this constitutes a significant health care burden, particularly for people of working age.1
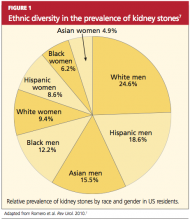
Nephrolithiasis is currently more prevalent in men than in women (13% vs 7%, respectively), and it is three to four times more likely to present in white than nonwhite patients.2 However, recent epidemiologic data suggest an alarming increase in the number of women and adolescents primarily diagnosed with stone disease.3-6 The pattern of increasing incidence in women can be attributed in part to changes in diet and lifestyle.4,5 Figure 17 represents the prevalence of stone disease, specific to gender and race.2,4
Due to kidney stones’ relatively common occurrence, the diagnosis, management, and prevention of stone disease have become increasingly relevant for the primary care practitioner. In the course of stone disease management, the clinician should be aware of a vital fact: Stones have a tendency to recur.1 Indeed, evidence suggests that following an initial diagnosis of nephrolithiasis, the probability of kidney stone recurrence increases to nearly 50% after five years.8
Even more concerning, evidence from several studies suggests that patients with a history of stone disease have a higher probability of experiencing a significant reduction in renal function (ie, decrease in glomerular filtration rate) and hence end-stage renal disease, when compared with non–stone formers.9-11 This accentuates the importance of early diagnosis, treatment, and initiation of steps to prevent further recurrence of this condition.
PATHOGENESIS
Stones in the urinary tract develop under specific urinary conditions, including supersaturation of the urine with stone-forming ions (ie, calcium, oxalate, uric acid, and phosphate) and deficiency of urinary stone inhibitors (citrate, magnesium, zinc, macromolecules, and pyrophosphate). Stone formation occurs in a mucoprotein matrix that attaches to the renal epithelium. Urine becomes supersaturated as a result of increasing levels of solutes (such as the stone-forming ions) and/or decreasing free water volume. When the concentration of stone-forming ions exceeds solubility in the urine (equilibrium solubility product), these ions can combine to form crystals.12,13
Stones are typed based on the ion composition of their crystals (see Table 12,12).
Once crystals are formed, they can also aggregate with other crystals, developing into a calculus.12 Urinary pH influences ion crystallization: Alkaline urine favors formation of calcium and/or phosphate stones, whereas acidic urine favors uric acid and cystine stone formation.13
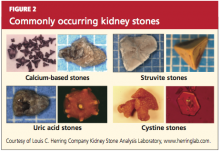
Kidney stones can be divided into four broad types: calcium-based, struvite, uric acid, and cystine stones (see Figure 2). Among these, calcium-based stones are by far the most common, with nearly 80% of stones composed of calcium compounds (usually calcium oxalate, and rarely calcium phosphate).4 The etiologies of these four types are vastly different, and prevention of stone formation must be tailored to the stone type. Once stones form, however, the appropriate treatment strategies have many similarities.
RISK FACTORS
Specific risk factors for stone formation vary widely and are unique to the type of stone. A thorough history, including a family or personal history of stone disease and dietary history, must be part of the initial work-up when a patient is being evaluated for stone disease; patients with any of these risk factors should be investigated further.
The risk factors for stone disease can be broadly categorized as either individual risk factors or dietary risk factors.
Individual Risk Factors
A positive family history increases the risk for stone formation by two- to three-fold. Other individual risk factors include congenital anatomic defects, such as medullary sponge kidney, horseshoe kidney, and ureteropelvic junction obstruction (UPJ).14-16 These can cause obstruction that leads to urinary stasis, and subsequently to stone precipitation.
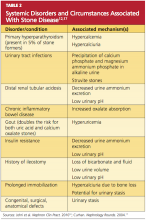
Certain systemic disorders (eg, hyperparathyroidism) and situations have also been associated with stone disease and should be considered risk factors. (See Table 212,17).
In patients who undergo gastrointestinal bypass surgery, the development of hyperoxaluria, hypercalciuria, and decreased urinary volume are associated with an increased risk for stone formation,18,19 and these patients should be watched for this development. Obesity and weight gain are directly proportional to nephrolithiasis risk, especially in women.4,20
Environment plays a very important role in stone formation. Persons who live in a hot, arid climate, for example, and those who work outdoors in hot weather are at increased risk for stone formation due to excessive fluid loss from sweating.2,4,7 (In regions where the risk for kidney stone formation is high, Romero et al7 predict, nephrolithiasis incidence could rise from 40% to 56% by 2050 as a result of the effects of global warming.)