Radiation Therapy
The goal of RT for men with localized prostate cancer is to deliver a therapeutic dose of radiation to the tumor while minimizing radiation to adjacent healthy tissues. Because of the prostate’s close anatomic proximity to the bowel, rectum, and bladder, the most common complications of RT are due to damage from radiation to surrounding structures in the gastrointestinal and genitourinary tracts.
Several forms of RT are available, including external beam radiation and brachytherapy. Radiation combined with hormonal therapy in high-risk patients has significantly improved outcomes, compared with men undergoing radiation alone.53Conformal 3D technology allows radiation oncologists to pinpoint the prostate and follow minute motion of the gland. This technology has helped to decrease the adverse effects of periprostatic radiation exposure.5,16Intensity-modulated radiation therapy offers increased accuracy in radiation dosage, improving cancer cure rates. External beam RT is used as adjuvant therapy in men with advanced disease and as salvage therapy for selected men who experience a rising serum PSA after RP.7,54
Brachytherapy involves the placement of radioactive seeds into the prostate under ultrasound guidance. It is an option for patients with low-risk prostate cancer and is performed as an outpatient procedure.5
Treatment for Disseminated Disease
Among men with disseminated disease, bone metastases are most common. Androgen deprivation therapy (ADT) is used to control the disease while maintaining the patient’s quality of life.2 Once prostate cancer no longer responds to this treatment, it is referred to as hormone-refractory prostate cancer.
Chemotherapy with docetaxel has been shown to extend survival in patients with hormone-refractory prostate cancer.2 Cabazitaxel is a new chemotherapy agent recently approved for use in combination with prednisone for the treatment of patients with metastatic hormone-refractory prostate cancer previously treated with a docetaxel-containing regimen.55,56
Currently, a large phase 3 clinical trial, led by the Cancer and Leukemia Group B,57 is under way to examine the addition of bevacizumab to docetaxel and prednisone for possible improvement in overall prostate cancer survival.2
Adverse Effects of Treatment
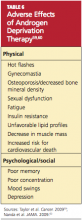
As successful as treatments for prostate cancer can be, they are not without significant adverse effects. Their severity varies by treatment plan and by patient, but they usually include physical and psychological effects. Men with prostate cancer are often less satisfied with the management of their disease than are other cancer patients.58 Adverse effects that they find particularly troublesome include urinary incontinence, erectile dysfunction, and effects associated with ADT (see Table 659,60).
Urinary incontinence is a resulting feature of both surgery and RT. After RP, men may have varying degrees of incontinence, ranging from stress incontinence to complete loss of urinary control. Incontinence usually improves within six to 12 months following surgery, with 2% to 22% of men experiencing long-term incontinence.5
Toxic effects of RT can occur immediately or after many years.5 Radiotherapy can result in cystitis, which usually develops a few weeks into treatment and improves after treatment is completed. Approximately one-half of patients who undergo RT experience urinary frequency, dysuria, or urgency due to cystitis, urethritis, or both. Long-term effects of radiation include persistent cystitis or urethral strictures.
Brachytherapy is associated with urinary symptoms that may take several weeks to develop. The side effects may be long lasting and can lead to obstruction of the urethra and urinary retention. Patients should be counseled to avoid bladder irritants, such as tea, coffee, alcohol, and carbonated beverages.
Reports of acute radiation proctitis vary from 2% to 40% of treated men.5,58 If the pelvic lymph nodes are within the treatment field, radiation enteritis may also be observed. Symptoms can include abdominal cramping, tenesmus, urgency, and frequent defecation. These can usually be controlled with antidiarrheal agents or topical anti-inflammatory preparations. Acute symptoms usually subside within three to eight weeks of RT completion. Long-term intestinal side effects persist in up to 10% of patients; these include diarrhea, tenesmus, rectal urgency, or hematochezia. Rectal or anal strictures, ulcers, and perforations are rare.5
Erectile dysfunction is the most common long-term adverse effect of RP, with reports of affected men (who have been advised to abstain from sexual intercourse for six to eight weeks following RP) ranging from 20% to 90%.5,52,61 Maximal recovery usually takes one to two years. Laparoscopic nerve-sparing surgeries have been developed to reduce the risk for erectile dysfunction.5,16,52
Thirty percent to 45% of men who were sexually potent before RT became impotent afterward, with frequency increasing over time.5,58 Factors that contribute to posttreatment impotence in this population include increasing age, intercurrent disease (eg, hypertension, cardiovascular disease, diabetes), and use of ADT.
Research among prostate cancer survivors and their spouses reveals that erectile dysfunction is the most important quality-of-life issue for the 50-to-64 age-group.62 Some men will recover a presurgical level of function, while others may require lengthy treatments, including surgical interventions, that may yield little or no success. Erectile dysfunction can be treated with PDE-5 inhibitors, penile injection therapy, vacuum erection devices, and penile prosthesis implantation.61