Additionally, stress-induced ST-T wave changes do not accurately localize the site of myocardial ischemia and provide no direct information on left ventricular function and other clinically important variables. The sensitivity and specificity of exercise ECG testing ranges from approximately 67% to 72%, which is below that of stress imaging techniques, whose average sensitivity ranges from 80% to 85%.7-9
Stress imaging modalities
For a patient with an abnormal resting ECG, evidence of left ventricular dysfunction, or a prior coronary revascularization, stress imaging with either echocardiography or nuclear perfusion scanning is appropriate. Both techniques show higher specificity than the stress ECG alone.
Nuclear imaging. Nuclear imaging uses radiotracers (thallium-201, technetium-99m tetrofosmin [Myoview], or technetium-99m sestamibi [Cardiolite]) to evaluate myocardial perfusion and function, and has greatly advanced the ability to detect and assess the extent of CHD. Stress myocardial perfusion imaging has a sensitivity of >90% for detecting patients at risk of cardiac death or MI.6
To detect ischemia or infarction, a radioisotope is injected at rest and after stress to produce images of myocardial regional uptake, which is proportional to regional blood flow. Normally, with maximal exercise or pharmacologic stress, myocardial blood flow is greatly increased above the resting condition. If a fixed coronary stenosis is present, myocardial perfusion in the territory supplied by the stenosis cannot be increased, which will create a flow differential and uneven distribution of the tracer.
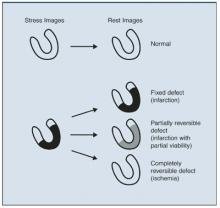
As illustrated in Figure 2, a normal myocardial perfusion image shows homogenous accumulation of radiotracer on both the stress and rest images. A perfusion defect appears as an area of reduced tracer uptake.
Nuclear perfusion studies can also provide a measure of left ventricular function and wall motion utilizing a bolus injection of radiotracer. While images can be obtained in most patients utilizing current techniques, artifacts due to breast and diaphragmatic tissue attenuation can lead to false-positive interpretation, particularly when examining women and when using thallium.
Echocardiography. Echocardiography visualizes the heart directly in real time using ultrasound, providing convenient assessment of the cardiac chambers, myocardium, valves, pericardium, and great vessels. The test can also identify mechanical complications of acute myocardial infarction, differentiate causes of reduced cardiac output and blood pressure, and help guide therapy. Stress echocardiography (exercise or pharmacologic stress) can be used to detect the presence, location, and severity of inducible myocardial ischemia as well as for risk stratification and prognosis.
During stress-induced ischemia, decrements in contractile function are directly related to decreases in regional subendocardial blood flow. Wall-motion changes precede ischemic ECG changes, accounting for the increased sensitivity of echocardiography versus ECG stress testing.
Interpretation of stress echocardiograms is based on analysis of segmental wall motion before and soon after stress. Normally, with exercise, or dobutamine infusion, left ventricular wall motion becomes hyperdynamic. The hallmark of ischemia is the development with stress of new, or the worsening of preexisting, wall motion abnormalities. The lack of improvement with stress in an already hypokinetic segment indicates infarction. Stress-induced left ventricular cavity enlargement, systolic dysfunction, or mitral regurgitation may also suggest CHD. Accuracy of stress echocardiography is similar to that of nuclear stress testing.
Considerable expertise in echocardiography is needed to rapidly acquire diagnostic images, so that its selection is limited by the skill of the technician. Image quality can be compromised by obesity and other factors, but the widespread use of intravenous contrast agents has significantly reduced the proportion of patients with uninterpretable images.
FIGURE 2
Accumulation of radiotracer in nuclear imaging (stress and rest images)
Patients who are not expected to achieve an adequate exercise capacity (as in our patient with osteoarthritis) should undergo pharmacologic stress testing with adenosine, dipyridamole, or dobutamine. Atrial pacing utilizing a swallowed esophageal electrode is also used in some cases. These agents, combined with echocardiographic or nuclear imaging, are particularly useful in patients who are unable to exercise adequately.
Pharmacologic stress agents are sometimes combined with low-level exercise protocols which may reduce the noncardiac side effects and improve image quality.10
Adenosine is the pharmacologic agent used most commonly in nuclear perfusion stress testing. An intravenous infusion of adenosine produces coronary vasodilation which is quickly attenuated when the infusion is terminated. Side effects, which are short-lived, include flushing, palpitations, and chest pain.
Dipyridamole is used less commonly due to its prolonged side effects and reports of lower specificity.11 Dobutamine, a beta-adrenergic agonist, increases heart rate and contractility in a dose-related fashion when infused intravenously. This agent is most commonly used in echocardiographic imaging. It can also be utilized with nuclear imaging when adenosine is contraindicated due to severe pulmonary or cerebrovascular disease. Side effects include transient arrhythmias, hypertension or hypotension, tremor, and chest pain.