Recent advances in treatment appear to have reversed the course of melanoma mortality since 2013, according to data published in the American Journal of Public Health.
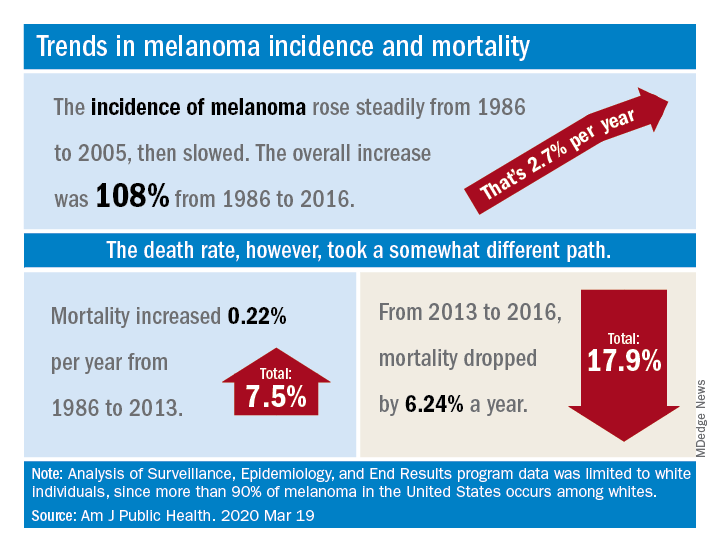
The U.S. death rate for melanoma, which had been rising at a rate of 0.22% a year for more than 2 decades, dropped by 17.9%, or 6.24% per year, during 2013-2016. That decline “coincides with the introduction of multiple new and efficacious treatments for metastatic melanoma,” such as BRAF inhibitors and immune checkpoint inhibitors, study author Juliana Berk-Krauss, MD, of the State University of New York Downstate Medical Center in Brooklyn and colleagues wrote.
The other possible explanation for the decline in deaths, “education and early detection resulting in migration toward earlier stage melanomas with a greater chance of surgical cure,” is unlikely, according to the investigators. That’s because the small decrease in median tumor thickness that occurred during 1989-2009 “is not associated with changes in prognosis.”
The investigators’ analysis encompassed data from the Surveillance, Epidemiology, and End Results registry recorded during 1986-2016. Nine registry areas were included (Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah), which covered about 9.4% of the U.S. population. The analysis was limited to the white population, which accounts for more than 90% of melanoma cases in the United States.
The data showed a slight decline in annual percent change in melanoma incidence, from 3.24% for 1986-2005 to 1.72% for 2006-2016. However, over the whole period studied (1986-2016), melanoma incidence increased by 108%, or about 2.7% per year.
“Given the increased incidence of melanoma throughout this period and the lack of stage migration, these data strongly suggest that the mortality decline is due to the extended survival associated with these [newer] treatments,” the investigators wrote.
This study was funded by NYU Langone. Two investigators disclosed potential conflicts of interest, including relationships with Bio-Rad Laboratories, Novartis, Merck, and several other companies.
SOURCE: Berk-Krauss J et al. Am J Public Health. 2020 Mar 19. doi: 10.2105/AJPH.2020.305567.