Bipolar disorder shares with ADHD the core symptoms of hyperactivity, impulsive behavior, and difficulty completing tasks. Mania and ADHD can look very similar if symptoms are observed at a single point in time. Bipolar illness is, by definition, episodic and fluctuating, while ADHD is much more constant. In addition, bipolar illness exhibits significant variation in mood, while ADHD may or may not be associated with impaired mood regulation. Up to 20% of patients with bipolar illness also have ADHD.7
Anxiety and depressive disorders can also share symptoms with ADHD-I. These include distractibility, poor concentration, and, in the case of anxiety, rapid changes in train of thought. Sleep disturbance, past trauma, and current acute stressors may manifest as clinical anxiety or depression, or may interfere with concentration and attention independently. As with bipolar illness, clinicians must look carefully at the time course of symptoms, including the age of onset. Classically, mood disorders develop in adolescence or early adulthood, while ADHD always has manifestations in childhood. Inattention and distractibility will track with mood if they are caused by an affective illness, but will remain in ADHD even when the patient is euthymic. On the other hand, patients with ADHD frequently become frustrated or overwhelmed as a result of their difficulties with task completion and social function, a presentation which can mimic anxiety or depression.8
Substance use disorder and ADHD interact in multiple ways and can present one of the more challenging diagnostic tasks when assessing a patient with impaired attention or concentration. ADHD is a powerful risk factor for future substance use,9 while substance use can impair attention, induce impulsivity, and alter concentration. Further, the treatment of choice for ADHD (stimulant medication) has the potential for misuse. The presence of continuous symptoms across settings is crucial in determining the proper diagnosis of ADHD.
Other conditions. Patients with a learning disability can be inattentive due to their cognitive limitations, or it may be comorbid with ADHD. If an intellectual deficit is suspected, referral for cognitive testing can help clarify the diagnosis. Autism also may cause significant alterations in attention with both hyper-focus and distractibility being common, as they are in ADHD. Intermittent explosive disorder shares the core symptom of impulsivity, but includes aggression, which is not always seen in ADHD. Personality disorders (eg, borderline, narcissistic) may also be difficult to distinguish from ADHD. The key to differentiation is the identification of behavior patterns outside the realms of concentration and attention.7
KEY DIAGNOSTIC CRITERIA
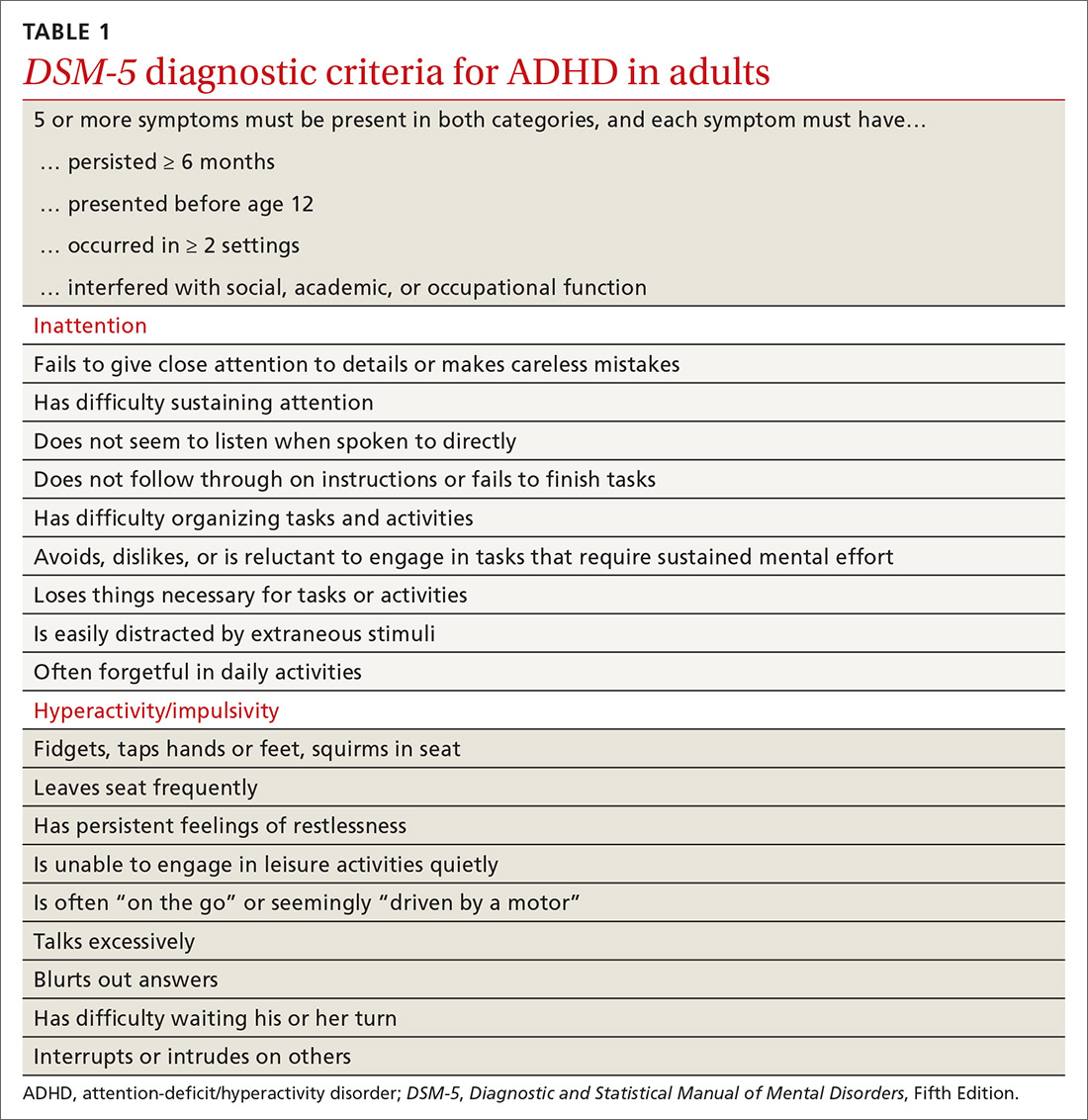
The diagnostic criteria for ADHD defined in DSM-5 are found in TABLE 1.1 Individuals ≥ 17 years old must meet 5 of 9 characteristics of inattention or 5 of 9 characteristics of hyperactivity/impulsivity (criterion A).1 Some symptoms must have been present prior to age 12 (criterion B). This cutoff is an increase from age 7 advised in DSM-IV.10 Symptoms must occur across at least 2 settings (criterion C) and significantly interfere with social, academic, or occupational functioning (criterion D). Exclusions include symptoms that occur exclusively in the context of a psychotic disorder or symptoms that are better explained in the context of other mental disorders (criterion E).1
Continue to: In the primary care setting