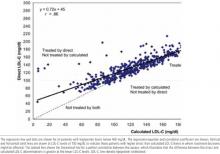
To determine whether triglyceride concentration influences treatment decisions by either method of LDL-C measurement, similar correlations and analyses were done on the data according to the following triglyceride groupings: <100 mg/dL, 100 to 199 mg/dL, 200 to 299 mg/dL, 300 to 399 mg/dL, and >400 mg/dL. This was further evaluated by plotting triglyceride vs D-LDL-C and triglyceride vs C-LDL-C (data not shown). Whereas the C-LDL-C showed no correlation with triglyceride, the DLDL-C showed a statistically significant correlation with triglyceride concentrations (r = .27), indicating that D-LDL-C increases at higher triglyceride levels. This suggested an influence of triglyceride on the D-LDL-C assay. This has been reported by others in 3 of 4 different D-LDL-C assays including the Sigma assay.15 However, alterations in treatment possibilities when using the D-LDL-C are present at all triglyceride concentrations.
FIGURE 1
Direct vs calculated LDL-C (mg/dL)
TABLE
Effect of LDL assay by LDL treatment cutoff*
| Patients who might be treated, n (%) | Additional patients who might be treated, n (%) | |||
|---|---|---|---|---|
| LDL cutoff for treatment, mg/dL | Calculated LDL | Direct LDL | Calculated, not direct, LDL | Direct, not calculated, LDL |
| >100 | 334 (72) | 393 (85) | 2 (<1) | 60 (13) |
| >130 | 185 (40) | 237 (51) | 2 (<1) | 55 (12) |
| >160 | 71 (15) | 87 (19) | 6 (1) | 21 (5) |
| *N = 464 patients. | ||||
| LDL, low-density lipoprotein. | ||||
Discussion
LDL-C has been identified in the NCEP-ATP III as the primary target of therapy. Treatment recommendations for high LDL-C are based on low, moderate, or high risk for CHD, with treatment goals of 160, 130, and 100 mg/dL, respectively.1,2
These evidence-based recommendations rely on data from clinical trials demonstrating prevention of CHD events by lowering LDL-C, all of which, with the exception of the recently reported Heart Protection Study, used the CLDL-C.18-23 Thus, important treatment decisions depend on this estimated LDL-C, and systematic deviations from the C-LDL-C will affect treatment decisions and cost.
The Sigma EZ LDL D-LDL-C assay in our hospital produces higher LDL-C levels than the C-LDL-C in a range of 100 to 160 mg/dL, the range of most common concern to clinicians. This results in inappropriate treatment or intensification in treatment according to the NCEP-ATP III guidelines. The DLDL-C was higher than the C-LDL-C at all triglyceride levels, but the error was greater for hypertriglyceridemia, the very situation for which it has been advocated.
Previous publications using a D-LDL-C assay have emphasized the correlation between the DLDL-C assay and research LDL-C determinations rather than the correlation with the C-LDL-C.5-8 Other investigators have observed a similar tendency for higher D-LDL-C than C-LDL-C measurements at an LDL-C of 100 mg/dL17 and a positive bias at higher triglyceride levels.14 Although C-LDLC was often performed, data similar to those shown in the Figure, ie, the simple correlation between the D-LDL-C and C-LDL-C, have not been presented. Two very recent reviews have suggested caution in routinely implementing the D-LDL-C assays and pointed out the considerable variation from one assay to another.14,15 Laboratories often change their assay method; in fact, our hospital laboratory has recently changed to a different DLDL-C method.
Physicians and institutions should be cautious about using a D-LDL-C method as a substitute for the C-LDL-C. First, it has not been standardized in large populations and, with the exception of the recent Heart Protection Study,23 has not been used in large clinical trials demonstrating the benefits of lowering LDL-C. Although the C-LDL-C has been recommended by the NCEP-ATP III,2 the Executive Summary of these guidelines did not address the method for measuring LDL-C.1 Second, cost is increased from the additional therapy and performing the D-LDL-C assay. Third, the major reasons proposed for using a D-LDL-C assay (lack of need for a fasting specimen and usefulness at triglyceride > 400 mg/dL) may not be valid or relevant. Variation in the LDL-C due to hypertriglyceridemia occurs with the D-LDL-C. In addition, the NCEP-ATP III report emphasized triglyceride and recommended a fasting lipid panel including total cholesterol, triglycerides, and HDL-C.1,2 One limitation of this study is the inclusion of predominantly male veterans. There may be populations, not considered in this study, that have an abnormal lipoprotein composition that significantly affects the C-LDL-C.
Conclusions
The C-LDL-C should remain the method of choice for LDL-C determinations because (1) this assay was used in clinical trials documenting the benefits of cholesterol-lowering therapy and (2) use of the D-LDL-C increases cost without evidence of benefit. Further studies are needed to standardize the direct LDL-C assays, and outcome trials using these assays need to be performed.
ACKNOWLEDGMENTS
This work was supported in part by the Biomedical Research Foundation of Arkansas and the Central Arkansas Veterans Healthcare System.