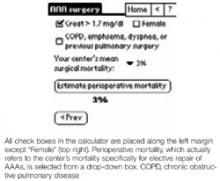
InfoRetriever’s final calculator, the algorithm by Steyerberg et al7 for elective repair of abdominal aortic aneurysms (AAA), is 2 screens comprising mostly check boxes. Drop-down menus are provided for age group (3 choices) and “Your center’s mean surgical mortality” (which should specify mortality for elective AAA repair), with choices from 3% to 12% (Figure 3). Steyerberg’s algorithm differs from the others in this review in that the intent is to predict total surgical mortality, not solely major cardiac risk. The focus is to help physicians assess and compare the operative risk of elective AAA repair with the reported natural history of nonoperative management of AAA, which may be particularly important in patients at advanced ages or with a limited life expectancy. No validation set is available for this index; the derivation set was 238 consecutive AAA patients enrolled from 1977 to 1988 from 1 institution in the Netherlands. It is unclear from the report7 whether the patients were enrolled prospectively. Until validated, we believe this decision aid needs to be cautiously applied.
FIGURE 3
InfoRetriever’s abdominal aortic aneurysm decision rule
Discussion And Conclusion
Based on our evaluation, we believe that few physicians will have detailed knowledge of the pertinent literature and the expertise to apply these risk indices accurately. However, the electronic implementation of the indices simplifies carrying them to the bedside. In our opinion, their main use is as checklists that serve as reminders of independent risk factors for adverse perioperative cardiac outcomes.
A major enhancement to each of these programs would be the addition of an opening screen that explained to which patients the program should be applied. However, the algorithmic preoperative management tools are well suited to the electronic and clinical environment.
Because the ACC/AHA decision support tool is newer (2002), we prefer it to the ACP tool (1997). STAT CC’s implementation is straightforward, occupies only 97K, and is free. For physicians who wish a low-, intermediate-, and high-risk classification, we recommend using Eagle’s 5-point, 3-class (0, 1–2, 3 points or more), easy-to-memorize scale (age >70, angina, prior MI [by history or ECG Q-waves], diabetes mellitus, congestive heart failure)—and forget the electronics.#
We believe an index such as the Detsky could (and should) be adapted for handheld computers, but the implementation of the versions we reviewed lack the features necessary for general utility. Such a version requires not only an explanation of angina classes, but also entry of pretest probability, specifically surgical risk for the surgical type. Many potential users probably will not know their institutions’ risk numbers for specific surgical types. Therefore, users should be assisted with estimating this entry based on literature values and suggestions about altering those values for the specific situation. While we like Steyerberg’s concept of estimating operative versus nonoperative mortality in AAA clinical decision-making, we await validation of this index.