- Do steroids change the course of Bell’s palsy?
- What is the role of surgery for Bell’s palsy?
- Should antiviral therapy be initiated for all patients?
Recommendations for these management issues are found in the guideline that was funded and developed by the American Academy of Neurology. Their Quality Standards Subcommittee, Practice Committee, and Board of Directors approved the recommendations. The target audience is physicians.
Patients with Bell’s palsy are the target population of this guideline. The objective is to summarize evidence regarding effectiveness of steroids, acyclovir, or surgical facial nerve decompression for improved functional outcomes in facial nerve palsy (Bell’s palsy). The evidence categories for this guideline are therapeutic effectiveness and treatment. Outcomes considered are 1) relative rate and 95% confidence interval for goodreturn of facial function, and 2) relative rate and 95% confidence interval for completereturn of facial function. The rating scheme is updated to comply with the SORT taxonomy.1
Guideline relevance and limitations
Bell’s palsy results from damage to the 7th (facial) cranial nerve and affects 40,000 Americans each year. It is seen commonly in pregnant women and diabetics, as well as those with viral illnesses. Besides facial paralysis, other symptoms of Bell’s palsy may include pain, hypersensitivity to sound in the affected ear, and impairment of taste. The common cold sore viruses, herpes simplex virus, and other herpes viruses are the likely pathogens causing many cases of Bell’s palsy. The prognosis for Bell’s palsy is good and most patients get better within 2 weeks. Over 80% recover facial nerve function within 3 months.2
A lengthy bibliography accompanies the guideline. The guideline is weakened by lack of a cost-effectiveness analysis.
Guideline development and evidence review
The authors searched the National Library of Medicine’s Medline database from 1966 to June 2000. The resultant prospective studies for treatments with steroids, acyclovir, or surgery were screened for outcome evidence. There are 25 references. A meta-analysis of patient data and a systematic review of the evidence were performed. Quality and strength of evidence were weighted according to a rating scheme.
Grade B Recommendations
- Treatment with oral corticosteroids improves facial function.
- Treatment with acyclovir, combined with steroids, improves facial function.
Grade C Recommendations
- Facial nerve decompression does not improve facial function.
Source for this guideline
Grogan PM, Gronseth GS. Practice parameter: Steroids, acyclovir, and surgery for Bell’s palsy (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2001; 56:830–836.
Other guidelines on bell’s palsy
- Assessment: Neurologic risk of immunization. Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology.
This older guideline refers to a few cases of Bell’s palsy associated with the plasma-derived hepatitis B vaccine used from 1982 to 1988. Since then the recombinant product has replaced the plasma-derived vaccine.
Source: Fenichel GM. Assessment: Neurologic risk of immunization: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology1999; 52:1546–1552. [30 references]
CORRECTION
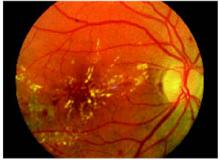
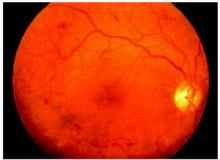
The photographs in the Figure appearing in last month’s Clinical Inquiry, “Do routine eye exams reduce occurrence of blindness from type 2 dia-betes?” (page 733), were transposed. They appear correctly below.
Correspondence
Keith B. Holten, MD, Clinton Memorial Hospital/University of Cincinnati Family Practice Residency, 825 W. Locust St., Wilmington, OH, 45177. E-mail: keholtenmd@cmhregional.com.