• Initiate beta-blocker therapy in low doses for patients with heart failure, and increase the dose gradually until the target dosage is achieved. A
• The benefit of beta-blocker therapy for patients with heart failure is proportional to the degree of heart rate reduction. A
• Consider beta-blocker therapy for patients with coexisting chronic obstructive pulmonary disease or decompensated heart failure, although treatment may have to be reduced or temporarily withheld. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
The evidence is clear: Beta-blockers reduce mortality and hospitalization in patients with systolic heart failure.1-3 Yet this class of drugs is underutilized by physicians who fear that beta-blocker’s negative inotropic effect will lead to worsening heart failure.4
Our aim in presenting this review is to counter such concerns by detailing the latest evidence. We draw on current research findings to answer questions about beta-blocker selection and dosage and address common misconceptions.
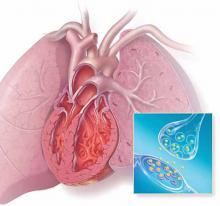
Beta-blockers shown blocking the effects of epinephrine and norepinephrine at the receptor sites.
Do beta-blockers lower mortality rates for patients with heart failure?
Yes. Three beta-blockers—bisoprolol, carvedilol, and metoprolol succinate—have been conclusively shown to reduce morbidity as well as mortality in patients with systolic heart failure (TABLE 1).1-3,5,6 Here’s a look at the studies:
Bisoprolol. The Cardiac Insufficiency Bisoprolol Study (CIBIS II), a randomized controlled trial (RCT) involving 2647 patients with New York Heart Association (NYHA) Class III or IV heart failure and an ejection fraction (EF) ≤35%, found that bisoprolol reduced the primary end point of all-cause mortality (hazard ratio [HR]=0.66; 95% confidence interval [CI], 0.54-0.81; P<.0001) compared with placebo. Cardiovascular mortality rates (HR=0.71; 95% CI, 0.56-0.90; P=.0049) and hospitalization rates (HR=0.80; 95% CI, 0.71-0.91; P=.0006) were significantly reduced, as well.1
Carvedilol. In the Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) trial, an RCT featuring 2289 patients with EF <25%, carvedilol significantly reduced the total death rate (HR=0.65; 95% CI, 0.52-0.81; P=.0014) compared with placebo.2
Metoprolol succinate. The Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF), a study of nearly 4000 patients with Class II to IV heart failure and EF ≤40%, found that metoprolol succinate lowered total mortality or all-cause hospitalization (HR=0.81; 95% CI, 0.73-0.90; P<.001) compared with placebo.3
TABLE 1
Beta-blockers for heart failure patients: What the studies show
| Trial | Study group (N) | Mean follow-up | Agent tested | Primary end point | RR; 95% CI; P value |
|---|---|---|---|---|---|
| BEST5 | Class III-IV HF, EF ≤35% (2708) | 2 y | Bucindolol | All-cause death | 0.90; 0.78-1.02; .13 |
| CIBIS II1 | Class III-IV HF, EF ≤35% (2647) | 1.3 y | Bisoprolol | All-cause death | 0.66; 0.54-0.81; <.0001 |
| COPERNICUS2 | HF symptoms, EF ≤25% (2289) | 10.4 mo | Carvedilol | All-cause death | 0.65; 0.52-0.81; .0014 |
| MERIT-HF3 | Class II-IV HF, EF ≤40% (3991) | 1 y | Metoprolol succinate | Composite* | 0.81; 0.73-0.90; <.001 |
| SENIORS6 | Age >70 y and hospitalization for HF or EF ≤35% (2128) | 21 mo | Nebivolol | All-cause death and CVD hospitalization | 0.86; 0.74-0.99; .039 |
| *All-cause mortality and all-cause hospitalization. BEST, Beta-blocker Evaluation of Survival Trial; CI, confidence interval; CIBIS II, Cardiac Insufficiency Bisoprolol Study; COPERNICUS, Carvedilol Prospective Randomized Cumulative Survival; CVD, cardiovascular disease; EF, ejection fraction; HF, heart failure; MERIT-HF, Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure; RR, relative risk; SENIORS, Study of the Effects of Nebivolol Intervention on Outcomes and Rehospitalisation in Seniors with Heart Failure. | |||||
Carvedilol and metoprolol go head-to-head
Although carvedilol and metoprolol have been shown to have similar hemodynamic and heart rate effects, the Carvedilol or Metoprolol European Trial (COMET) found that carvedilol is superior in extending survival. More than 3000 patients with Class II to IV heart failure and an EF <35% were randomized to carvedilol (target dose 25 mg bid) or metoprolol tartrate (target dose 50 mg bid). After 58 months, total mortality was significantly lower in the carvedilol arm (HR=0.83; 95% CI, 0.74-0.93; P=.0017).7
Which metoprolol formulation? While RCTs have found that metoprolol tartrate has a favorable effect on EF and hemodynamic data, it is not approved by the US Food and Drug Administration (FDA) as a treatment for heart failure—and its ability to reduce morbidity and mortality in patients with heart failure has not been established.8,9 Thus, metoprolol succinate, but not metoprolol tartrate, is recommended for heart failure treatment by the American College of Cardiology, American Heart Association, and European Society of Intensive Care Medicine.10,11
These agents lack evidence of efficacy
Not all beta-blockers have therapeutic value for patients with heart failure—or evidence to support them.
Bucindolol. The Beta-blocker Evaluation of Survival Trial (BEST), a trial of 2708 patients with Class III or IV heart failure and an EF ≤35%, found no difference in total mortality between bucindolol and placebo.5 As a result, the drug did not receive FDA approval.12 The FDA has since designated the investigation of bucindolol (trade name Gencaro) for the reduction of cardiovascular hospitalizations and mortality of heart failure patients with a particular genotype as a Fast Track development program.13