The 1999 BRFSS questions regarding use of sigmoidoscopy were modified from previous questionnaires. As the scientific evidence supporting CRC screening tests has grown, BRFSS CRC survey questions have changed. The 1997 survey, described previously,12 was the first survey to collect information regarding the use of home-administered FOBT and sigmoidoscopy from all 50 states, the District of Columbia, and Puerto Rico. In 1997, respondents were asked if they had received a sigmoidoscopy or proctoscopy. Proctoscopy, performed with a shorter instrument than a sigmoidoscope, is not recommended as a CRC screening test. In 1999, the term “sigmoidoscopy/proctoscopy” was replaced with “sigmoidoscopy/colonoscopy.” Colonoscopy evaluates the entire colon and is recommended once every 10 years in some guidelines.10,11 For this report, the terms “sigmoidoscopy/proctoscopy” and “sigmoidoscopy/colonoscopy” will each be referred to as “sigmoidoscopy” unless otherwise specified.
TABLE 1
Questions used in the 1999 Behavioral Risk Factor Surveillance System to assess usage of colorectal cancer screening tests
|
Results
The age-adjusted proportion of overall respondents who reported ever receiving CRC screening tests in 1999 was 40.3% for FOBT and 43.8% for sigmoidoscopy (data not shown).
The 1999 age-adjusted CRC screening test rates are presented by demographic subgroups for reported use within recommended time intervals: FOBT within the year preceding the survey, sigmoidoscopy within the past five years, or at least one of the two tests (Table 2). Less than half of the population surveyed reported having either FOBT or sigmoidoscopy within the recommended time interval. In 1999, 20.6% of respondents reported having had FOBT within the previous year; 33.6% reported having had a sigmoidoscopy within the previous 5 years; 44.0% reported having had either FOBT within the previous year or a sigmoidoscopy within the previous 5 years. There was little difference in test use between blacks and whites. Rates of use by Asian/Pacific Islanders and American Indian/Alaska Natives were calculated from small respondent samples and should be interpreted cautiously. Respondents of Spanish or Hispanic origin reported lower rates of FOBT and sigmoidoscopy than respondents who were not of Hispanic origin. Reported test use rose with increasing age of the respondents, up to age 70–79, and then declined for those over 80 years of age. Reported test use increased with education and with annual house hold income. Respondents who had health care coverage were almost twice as likely to have had CRC screening tests as respondents without health care coverage.
CRC screening test rates increased slightly from 1997 to 1999. In 1997, 19.6% of respondents reported having had an FOBT within the previous year and 30.3% reported having had a sigmoidoscopy within the previous 5 years.
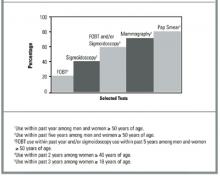
We compared 1999 BRFSS usage rates for FOBT and sigmoidoscopy or colonoscopy with those for mammography and Papanicolaou (Pap) smear (Figure). These are not direct comparisons but, rather, comparisons of the rates of testing within recommended time intervals among appropriate demographic groups. The proportion of persons who used CRC screening tests within recommended time intervals was lower than those for other cancer screening tests.
TABLE 2
Respondents aged 50 years or older who reported colorectal cancer screening tests within recommended time intervals, by demographic variables1
| Fecal occult blood test within previous year | Sigmoidoscopy/colonoscopy within previous 5 years | Either test within recommended time interval | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n2 | % | (95% CI) | n | % | (95% CI) | N | % | (95% CI) | |
| Total | 61,952 | 20.6 | (20.1–21.2) | 61,953 | 33.6 | (33.0–34.2) | 61,537 | 44.0 | (43.3–44.6) |
| Gender | |||||||||
| Male | 23,919 | 19.1 | (18.2–19.9) | 23,850 | 37.9 | (36.8–38.9) | 23,724 | 45.9 | (44.9–47.0) |
| Female | 38,033 | 22.0 | (21.3–22.7) | 38,103 | 30.4 | (29.6–31.1) | 37,813 | 42.6 | (41.7–43.4) |
| Race4 | |||||||||
| White | 55,139 | 21.0 | (20.5–21.6) | 55,170 | 33.6 | (33.0–34.3) | 54,804 | 44.2 | (3.5–44.9) |
| Black | 4,075 | 20.7 | (18.8–22.6) | 4,046 | 32.6 | (30.3–34.9) | 4,020 | 43.3 | (40.9–45.7) |
| Asian/Pacific Islander | 739 | 10.3 | (6.9–13.6) | 739 | 35.4 | (28.4–42.5) | 735 | 40.1 | (33.3–46.9) |
| American Indian/ Alaska Native | 725 | 18.2 | (12.7–23.7) | 725 | 36.0 | (29.4–42.5) | 723 | 43.0 | (36.5–49.6 |
| Spanish or Hispanic origin | |||||||||
| Yes | 3,664 | 11.2 | (9.4–12.9) | 3,667 | 28.6 | (25.6–31.5) | 3,635 | 33.9 | (30.9–37.0) |
| No | 57,993 | 21.4 | (20.9–21.9) | 57,999 | 34.0 | (33.4–34.6) | 57,620 | 44.8 | (44.1–45.5) |
| Age (group) | |||||||||
| 50–59 years | 23,758 | 15.5 | (14.7–16.2) | 23,803 | 26.1 | (25.1–27.0) | 23,667 | 34.7 | (33.7–35.7) |
| 60–69 years | 17,680 | 23.0 | (22.0–24.0) | 17,651 | 36.9 | (35.7–38.1) | 17,574 | 48.1 | (46.9–49.3) |
| 70–79 years | 14,427 | 25.8 | (24.6–27.0) | 14,412 | 40.7 | (39.3–42.1) | 14,306 | 52.7 | (51.4–54.1) |
| ≤80 years | 6,087 | 21.6 | (19.8–23.4) | 6,087 | 36.1 | (34.0–38.2) | 5,990 | 46.9 | (44.7–49.1) |
| Education | |||||||||
| < 12 years | 11,928 | 15.0 | (13.8–16.1) | 11,889 | 27.5 | (25.9–29.1) | 11,756 | 35.6 | (33.9–37.3) |
| High school graduate | 21,183 | 19.7 | (18.8–20.6) | 21,176 | 30.6 | (29.6–31.6) | 21,049 | 41.2 | (40.1–42.3) |
| Some college/ technical school | 14,167 | 23.5 | (22.3–24.7) | 14,162 | 35.9 | (34.6–37.3) | 14,102 | 47.9 | (46.5–49.2) |
| College graduate | 14,503 | 24.3 | (23.2–25.5) | 14,560 | 41.1 | (39.8–42.5) | 14,466 | 51.4 | (50.1–52.7) |
| Income (annual household) | |||||||||
| <$20,000 | 15,204 | 15.3 | (14.3–16.3) | 15,154 | 29.1 | (27.7–30.5) | 15,029 | 37.0 | (35.5–38.4) |
| $20,000–34,999 | 14,354 | 20.8 | (19.7–21.9) | 14,362 | 32.5 | (31.2–33.8) | 14,288 | 43.0 | (41.7–44.4) |
| $35,000–49,999 | 7,721 | 23.3 | (21.6–24.9) | 7,718 | 37.0 | (35.1–39.0) | 7,703 | 48.2 | (46.3–50.1) |
| ≥$50,000 | 11,967 | 24.2 | (22.7–25.6) | 12,002 | 41.7 | (39.9–43.4) | 11,949 | 51.7 | (50.0–53.5) |
| Health care coverage | |||||||||
| Yes | 57,551 | 21.3 | (20.8–21.9) | 57,561 | 34.7 | (34.1–35.4) | 57,169 | 45.4 | (44.7–46.1) |
| No | 4,331 | 12.1 | (9.8–14.5) | 4,326 | 18.7 | (15.6–21.7) | 4,304 | 25.7 | (22.2–29.2) |
| 1From the Behavioral Risk Factor Surveillance System (BRFSS), 1999; estimates are age-adjusted. | |||||||||
| 2Sample size for each question; sample sizes may not sum to totals because of missing data. | |||||||||
| 3Confidence interval. | |||||||||
| 4Sample sizes for racial categories do not add up to column totals. “Other” racial category not presented here. | |||||||||
FIGURE
Comparison of use of colorectal cancer screening tests with other screening tests, BRFSS 1999
Discussion
Currently, 4 widely accepted tests are available for CRC screening, and several new tests are under investigation.16,17 Not enough evidence exists to determine which of the available tests is most appropriate when efficacy, cost-effectiveness, availability, patient acceptability, and safety are taken into consideration. The 1999 BRFSS monitored the use of 3 of these tests: FOBT and sigmoidoscopy or colonoscopy. Our results show that less than half of the US population aged 50 years and older is being screened for CRC with these methods. Persons with health care coverage and with higher education and income levels were more likely to have had CRC tests. Since 1997, the proportion of the U.S. population being screened for CRC has increased slightly, but it remains low and lags far behind the use of other recommended cancer screening tests (Figure). While use of barium enema, one of the recommended colorectal cancer screening tests, is not monitored in the 1999 BRFSS, data from a recent national primary care physician survey suggest that barium enemas are infrequently recommended for colorectal cancer screening (Carrie Klabunde, National Cancer Institute, personal/written communication, 2002).