Diagnosis
- Chest radiography is useful (B).
- Spirometry should not be used to diagnose an exacerbation or to assess its severity (A).
- An arterial blood gas reading is helpful in gauging the severity of an exacerbation (A).
- There is little evidence regarding the contribution of additional laboratory testing, the predictive value of physical examination findings, or the usefulness of electrocardiography or echocardiography.
Treatment
- Inhaled short-acting beta-2 agonists and anticholinergic bronchodilators have positive effects. Since inhaled anti-cholinergic bronchodilators have fewer side effects, use them first. If improvement is slow with the initial bronchodilator, even at maximum dose, add a second bronchodilator (A).
- Parenteral agents (methyxanthines and sympathomimetics) are not as effective and have potential adverse effects (B).
- Mucolytic medications and chest physiotherapy are not effective (C).
- Systemic corticosteroids improve respiration and reduce relapse rate (A).
- Noninvasive positive-pressure ventilation decreases risk for invasive mechanical ventilation (A).
- Oxygen is beneficial for hypoxemic patients (B).
- Antibiotics are beneficial. Narrow-spectrum antibiotics (eg, amoxicillin, trimethoprimsulfamethoxazole, or tetracycline) are recommended as first-line agents. The more severe the episode, the more beneficial are antibiotics (A). There is no data regarding the optimal length of antibiotic treatment.
- Little evidence is available regarding the empiric use of diuretics.
Prognosis
- No methods reliably predict readmission to the hospital within 14 days after discharge (B).
- No methods reliably predict inpatient mortality (B).
Would you order a chest film to evaluate an acute exacerbation of chronic obstructive pulmonary disease (COPD)? Which medication would you first prescribe—a short-acting inhaled beta-2 agonist or an anticholinergic bronchodilator?
These are important questions for family physicians who commonly manage acute exacerbations of COPD.
The guideline summarized here was developed by a joint expert panel of the American College of Physicians–American Society of Internal Medicine and the American College of Chest Physicians. Three outcomes were considered: treatment efficacy, 6-month mortality, and relapse, as defined by return visit to the emergency department within 14 days of initial presentation. Systematic reviews with evidence tables were used to analyze data. The rationale for each recommendation is clear and well documented.
We added strength-of-recommendation ratings, which are not in the original guideline.
Limitations of the Guideline and Additional Evidence
Several weaknesses underlie this guideline. The authors found that, despite the importance of COPD, it has been the subject of very few high-quality studies. The highest-quality studies were few in number and had enrolled a small number of participants. The authors did not grade the strength of each recommendation in the summary document or in the detailed manuscripts, making it difficult to rapidly review.
Different diagnostic criteria are used in the source studies, making the context of treatment recommendations difficult to fully understand. Outcome endpoints also varied among studies. Goals for oxygen therapy were not addressed. Antibiotic treatment was based on studies before the emergence of multidrug-resistant organisms, particularly Streptococcus pneumoniae. It did not address tobacco use or smoking cessation, vaccine administration, outpatient management, management of stable COPD, or stratification of patients by severity.
Guideline Development and Evidence Review
Literature searches were performed using MEDLINE (1966–2000), EMBASE (1966– 2000), Health Star (1966–2000), and the Cochrane Controlled Trials Register (2000, Issue 1).
Search strategies included the index terms and text words chronic obstructive pulmonary disease and acute exacerbation and specific terms relating to interventions and outcomes. Variations on several search strategies were tested to locate the greatest number of relevant articles. Reference lists of retrieved articles were also examined. In all, 770 source articles were found.
Two other Guidelines for COPD
- Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Bethesda, Md: Global Initiative for Chronic Obstructive Lung Disease, World Health Organization/National Heart, Lung, and Blood Institute; 2001. Various pagings. (Web access at: www.goldcopd.com.)
- Veterans Health Administration (VHA). Clinical practice guideline for the management of chronic obstructive pulmonary disease. Version 1.1a. Washington, DC: Department of Veterans Affairs (US), Veterans Health Administration; 1999 Aug. 116 p. (Web access at: www.oqp.med.va.gov/cpg/COPD/ COPD_base.htm).
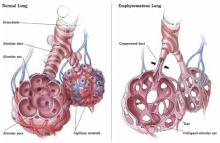
FIGURE
Emphysematous dysfunction in COPD
Correspondence
Keith B. Holten, MD, Clinton Memorial Hospital/University of Cincinnati Family Practice Residency, 825 W. Locust St., Wilmington, OH, 45177. E-mail: keholtenmd@cmhregional.com.