Success in the United States in reducing morbidity caused by syphilis and gonorrhea has been offset by the rising morbidity seen with other sexually transmitted diseases (STDs), such as chlamydia and herpes. Also, recent increases in the prevalence of syphilis and human immunodeficiency virus (HIV) underscore the fact that sustaining public health successes depends on constant surveillance and a commitment to control efforts.
This Practice Alert focuses on 3 prevalent STDs: syphilis, gonorrhea, and chlamydia—those patients most likely to be infected, and specific developments in screening, diagnosis, and treatment.
Those most likely to be infected
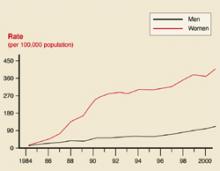
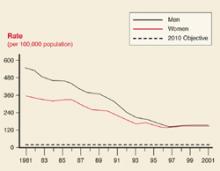
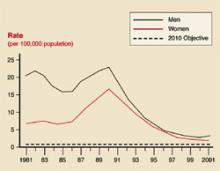
In 2001, 783,000 cases of chlamydia, 362,000 cases of gonorrhea, and 31,600 cases of syphilis were reported to the Centers for Disease Control and Prevention (CDC).1 The true incidence of each disease is unknown. Historical trends in the number of cases reported are reflected in Figures 1 ,2, and 3. In 2001, there was a slight increase in the number of syphilis cases, reversing a 10-year downward trend. The number of chlamydia cases continued to rise, which may reflect improved screening and reporting, while the number of gonorrhea cases continued downward.
FIGURE 1
Chlamydia rates
Chlamydia rates by sex: United States, 1984–2001.
FIGURE 2
Gonorrhea rates
Gonorrhea rates by sex: United States 1981–2001, and the Healthy People year 2010 objective.
FIGURE 3
Syphilis rates
Primary and secondary syphilis rates by sex: United States 1881–2001, and the Healthy People year 2010 objective.
Chlamydia
Infection with Chlamydia trachomatisis reported 4 times as often in women as in men, reflecting better screening of women in family planning programs and during prenatal care.2 The highest rates of chlamydia in women occur in the age groups 15 to 19 years (25/1000) and 20 to 25 years (24/1000). Testing in family planning clinics has yielded chlamydia infection rates of 5.6% among these women.2
Gonorrhea and syphilis
The age groups at highest risk for gonorrhea are 15 to 19 years for women (703/100,000) and 20 to 24 for men (563/100,000).3 For syphilis, the highest risk for women is age 20 to 24 years (3.8/100,000 for primary and secondary syphilis) and 35 to 39 years for men (7.2/100,000).4 There are marked geographic variations in the rates of syphilis (Figure 4). The recent increase in syphilis has been among men, largely attributed to homosexual activity.
FIGURE 4
Syphilis rates by county
Counties with primary and secondary syphilis rates above and below the Healthy People year 2010 objective: United States, 2001.
When and whom to screen
Many STDs persist asymptomatically. These silent infections can cause long-term morbidity such as infertility, pelvic inflammatory disease, ectopic pregnancies, and chronic pelvic pain. Both the United States Preventive Services Task Force and the American Academy of Family Physicians recommend that screening for STDs be performed in specific circumstances (Table 1).9,10
These recommendations should probably be considered a minimum standard, with other groups and diseases included based on the local epidemiology. The local or state health department can be a useful source of information on local epidemiologic patterns and screening and treatment recommendations. Keep in mind that the accuracy of local disease statistics depends on screening and disease reporting by local physicians.
TABLE 1
When and whom to screen for chlamydia, gonorrhea, and syphilis
| Chlamydia | Sexually active women aged 25 years should be routinely tested, and tested during pregnancy at the first prenatal care visit. |
| Other women at high risk* for chlamydia should be routinely tested, and tested during pregnancy at the first prenatal care visit. | |
| Gonorrhea | High-risk women* should be routinely tested, and tested during pregnancy at the first prenatal care visit |
| Syphilis | High-risk women should be routinely tested, and tested during pregnancy at the first prenatal care visit, again in the third trimester, and at delivery. |
| All pregnant women should be tested at the first prenatal care visit. | |
| * Definitions for high risk vary but generally include the following: those with multiple sex partners, other STDs, sexual contact to those with disease, or who exchange sex for money for drugs. | |
Urine screening tests
New nucleic acid amplification tests (NAAT) facilitate screening and diagnosis of chlamydia and gonorrhea with a urine sample. This offers the ease of urine collection in both men and women, with the added benefit of sensitivitiesand specificities equal to those obtained from urethral or endocervical samples. NAATs make possible urine screening in settings where urethral and cervical samples may not be possible because of logistics or patient nonacceptance.
NAATs do not require the presence of live organisms, and only a small number of organisms are needed for accurate test results.
One disadvantage of these tests is an inability to determine antibiotic sensitivities. Another is occasional false-positive results from dead organisms, which can occur if test of cures are performed too soon after treatment (less than 3 weeks).