A 60-year-old African American woman who had congestive heart failure (CHF) with reduced ejection fraction, untreated hepatitis C virus infection, and chronic kidney disease presented to the emergency department (ED) with a 6-month history of bilateral lower extremity edema. Use of diuretics and antibiotic therapy for suspected CHF exacerbation and cellulitis, directed by her primary care physician, had no effect. In the month prior to presenting to the ED, the patient took 2 different antibiotics, each for 10 days: clindamycin 300 mg every 6 hours and doxycycline 100 mg every 12 hours. Additionally, she was taking furosemide 40 mg/d with good urine output, but no appreciable improvement in lower extremity edema.
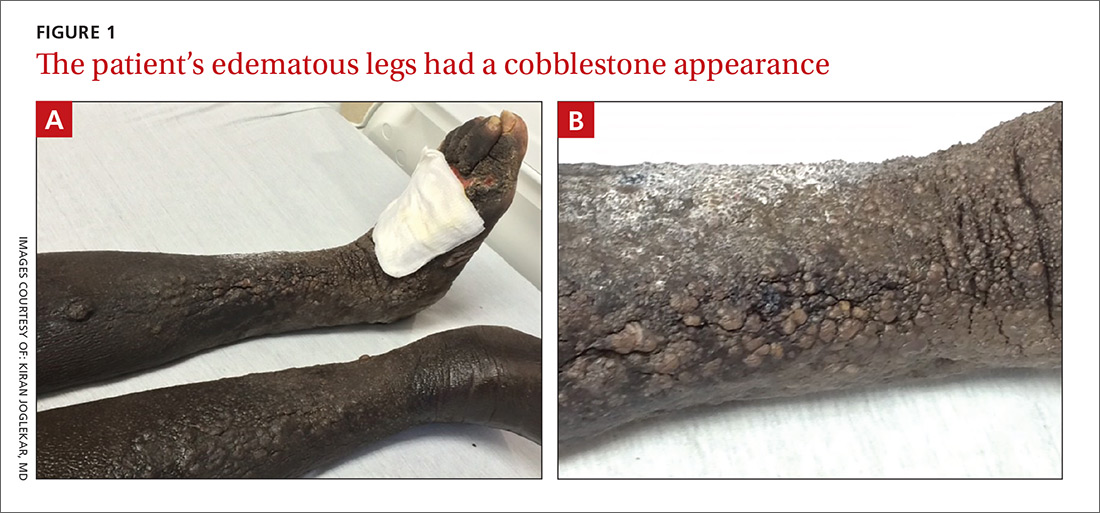
The physical examination revealed bilateral nonpitting edema. Weeping pearly papules, xerotic skin, and a cobblestone appearance extended from the dorsa of the patient’s feet to her knees (FIGURES 1A and 1B). The patient underwent Doppler ultrasound of the lower extremities and a skin biopsy.