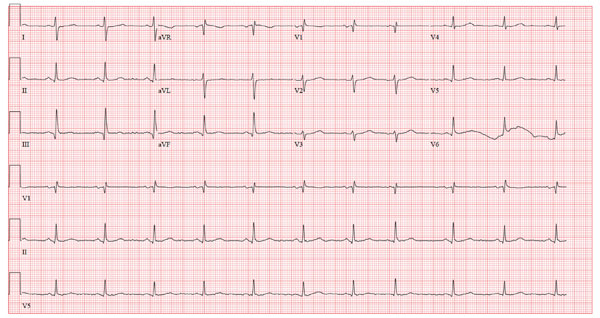
A 65-year-old man who lives in a remote village in Alaska is in your area on vacation. He presents to your office stating he has had a cold for the past three weeks that “just won’t go away.” He has tried several OTC medications without success, and he now has a productive cough. You notice as you walk into the examining room that it reeks of cigarette smoke. On questioning the patient, you learn that he has smoked two to three packs of cigarettes a day for most of his life. He is proud to announce that now he is down to 1.5 packs per day. He denies chest pain, fevers, chills, or night sweats, but admits that he is more short of breath than usual and has discomfort in his right chest. He can only walk 25 or 30 feet before he must rest, and he cannot climb one flight of stairs without stopping. He plans to return home in four days and is concerned that he won’t be able to function independently, stating, “You can die up there pretty easily if you’re not up to speed.” His medical history is remarkable for coronary artery disease with three-vessel coronary artery revascularization in 2004, paroxysmal atrial fibrillation, dyslipidemia, chronic obstructive pulmonary disease, and arthritis. Current medications include allopurinol, aspirin, atenolol, fluticasone-salmeterol and albuterol inhalers, folic acid, furosemide, isosorbide mononitrate, lisinopril, potassium chloride, rosuvastatin, and warfarin. He acknowledges that he does not take his warfarin routinely. He is allergic to codeine. Family history is remarkable for a father who died of a myocardial infarction at age 63, and two younger brothers who have had coronary revascularization procedures. He is a retired commercial fisherman who lives alone. He admits to drinking one six-pack of beer per day and occasionally smoking marijuana. A review of systems is remarkable for recurring headaches and a 10-lb weight loss over the past three months. The physical exam reveals a disheveled man in no distress. His blood pressure is 160/94 mm Hg; pulse, 70 beats/min; respirations, 18 breaths/min-1; and temperature, 100.4°F. His teeth are in poor repair, with multiple caries. The lungs reveal diminished vesicular breath sounds throughout with late inspiratory crackles in the right upper lung fields and few breath sounds with late expiratory wheezes in the right lower quadrant. The neck veins are flat, and there are no murmurs, rubs, or extra heart sounds. The abdomen is obese but benign, and there are no neurologic findings. Pertinent laboratory findings include a white blood count of 14,300/mm3 with 75% neutrophils, 20% bands, and 15% lymphocytes. A chest x-ray reveals normal cardiac size, sternotomy wires and surgical clips, and right lower-lobe consolidation consistent with right lower lobe pneumonia. An ECG shows the following: a ventricular rate of 65 beats/min; PR interval, 162 ms; QRS duration, 90 ms; QT/QTc interval, 448/465 ms; P axis, 60°; R axis, 101°; and T axis, 55°. What is your interpretation of this ECG?