Two days ago, a 76-year-old man underwent surgical repair of a left femoral fracture sustained in an automobile accident. Last night, his vital signs were concerning for asymptomatic bradycardia, prompting an order for ECG prior to morning rounds. His postoperative surgical course has been otherwise uneventful, and he is using minimal narcotic analgesia.
The patient has a long history of mild hypertension, which is well controlled with hydrochlorothiazide (50 mg/d). Otherwise, his medical history shows no angina, dyspnea, shortness of breath, or palpitations. There is no history of thyroid dysfunction or renal disease.
A pack-a-day smoker since age 15, the patient has been using a nicotine patch during his hospital stay. In the past 36 hours, he has taken 4 acetaminophen/oxycodone tablets (325/5 mg).
The patient works on a 400-acre ranch with about 100 head of cattle. His alcohol consumption was heavy until about 12 years ago, when he “blacked out” and gave up drinking altogether. He attends Alcoholics Anonymous meetings and leads sessions at his church. He denies recreational or illicit drug use.
Family history is positive for prostate cancer in his father and lung cancer in two brothers. His mother died of a hemorrhagic stroke at age 84.
The review of systems is remarkable only for discomfort due to an indwelling Foley catheter placed at the time of the surgery. He has no other specific complaints.
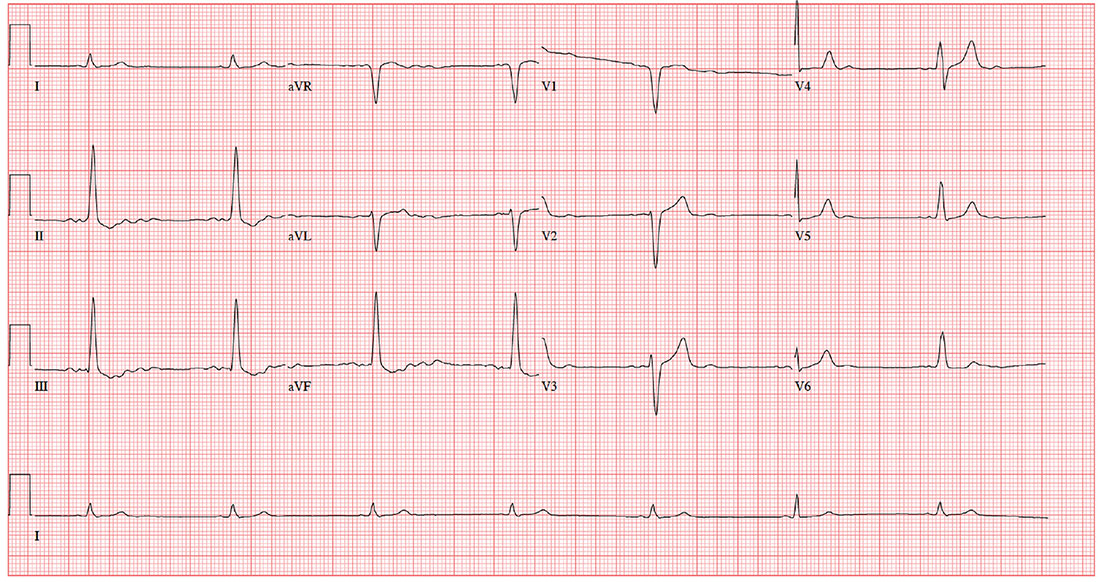
This morning, his vital signs include a blood pressure of 108/60 mm Hg; pulse, 42 beats/min; and O2 saturation, 100% on 2L of oxygen via nasal prongs.
When you arrive at the patient’s room, the ECG is in progress. The technician expresses concern about the tracing and shows you that the electrodes are placed properly. Looking at the ECG, you see a ventricular rate of 42 beats/min; PR interval, unmeasured; QRS duration, 130 ms; QT/QTc interval, 514/429 ms; P axis, +83°; R axis, +84°; and T axis, –43°. What is your interpretation?