Of the 1127 eligible patients, 1081 were included in the matched cohort, with 576 (53%) treated as hospitalized patients and 505 (47%) treated as outpatients. The mean age of the matched cohorts was 63.2 years for the inpatient group and 63.6 years for the outpatient group. Overall, the cohorts were well matched.
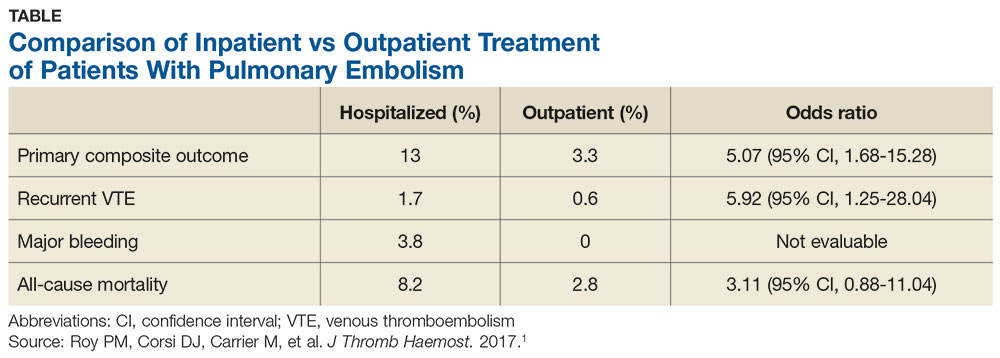
The 14-day rate of adverse events was higher in hospitalized patients than in outpatients (13% vs 3.3%; odds ratio [OR], 5.07), with each of the adverse events that made up the primary outcome occurring more frequently in the hospitalized group (see Table). The rate of adverse events at 3 months was also greater for hospitalized patients compared with outpatients (21.7% vs 6.9%; OR, 4.9). The results remained similar for high-risk patients (Class III-V) based on their PESI score.
WHAT’S NEW
Higher rate of adverse events in inpatients
This trial supports the CHEST guideline recommendations to manage hemodynamically stable patients with acute PE as outpatients.3 It adds to the conversation by demonstrating higher rates of adverse events with hospitalization, even in high-risk subgroups (PESI Class III-V).
CAVEATS
Good study, but it wasn’t an RCT
While this is a well-designed cohort study, it is not an RCT. This study defined outpatient management as patients discharged from the ED or hospitalized for < 48 hours. However, only 59 of the 544 patients in the outpatient group were early hospital discharges; the rest were never admitted. Finally, a specialized thrombosis clinic followed up with the patients within 24 hours of discharge, and patients had telephone access to specialized health care professionals; such organization of care contributed to the safe outpatient management of these PE patients.
CHALLENGES TO IMPLEMENTATION
Insurance coverage may present an issue
Medication coverage of direct oral anticoagulants and low-molecular-weight heparin may present a barrier to patients treated in the outpatient setting who have no insurance or are insured by certain carriers.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2018. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2018;67[12]:777-779).