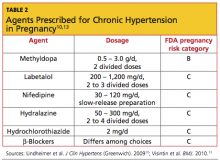
For chronic hypertension in pregnancy, the American Society of Hypertension10 has recommended several agents. There is no consensus on which medication is most appropriate (see Table 210,13).
Patient Education
Patient education is an important aspect of caring for women with PIH. The American Academy of Family Physicians29,30 provides a comprehensive patient education resource that defines the hypertensive disorders in pregnancy, explains the symptoms and signs of severe hypertension or preeclampsia, and describes appropriate diagnostic tests, monitoring, and treatment options. (See http://familydoctor.org/familydoctor/en/diseases-conditions/pregnancy-induced-hypertension.printerview.all.html.)
Patients who are considering pregnancy should be counseled to maintain a healthy weight prior to and during pregnancy. Adequate dietary calcium can reduce the risk for PIH, and calcium supplementation has been shown to reduce the risk for preeclampsia, especially in women at high risk.31 The Society of Obstetricians and Gynaecologists of Canada recommends low-dose aspirin (75 mg/d) at bedtime for high-risk women, starting before pregnancy, or upon diagnosis of pregnancy to prevent preeclampsia.6 Although there is insufficient evidence to recommend dietary salt restriction, excess salt can increase fluid retention and possibly blood pressure. Patients should be urged to attend all scheduled prenatal visits and to review the warning signs and symptoms of severe hypertension and preeclampsia at each visit.
Mode of delivery may be discussed and will depend on the severity of hypertension, presence of preeclampsia, and fetal well-being. Vaginal delivery at term is considered optimal unless there are indications for cesarean delivery. Induction of labor may be considered at term in patients with PIH. Those with severe preeclampsia who may require preterm delivery must be prepared for potential issues associated with prematurity.
Follow-Up and Prognosis
Patients with PIH should be evaluated postpartum for persistent hypertension. Blood pressure in patients with PIH usually normalizes by day 7 postpartum.32 If blood pressure elevation persists past 12 weeks postpartum, the patient’s diagnosis is revised to chronic hypertension and managed accordingly.
In the patient with persistent hypertension who chooses breastfeeding, it is important to select an antihypertensive medication with low transfer into breast milk. Many β-adrenergic antagonists and calcium channel antagonists are considered “compatible” with breastfeeding by the American Academy of Pediatrics.33
In addition to the potential for recurrent PIH in subsequent pregnancies, women with PIH are at increased risk for hypertension later in life, and findings from several large cohort studies suggest increased cardiovascular risk in patients with hypertensive pregnancies.16,34 Magnussen et al,9 who followed more than 15,000 mothers of singleton infants for several years postpartum, found that those who experienced hypertensive disorders (particularly recurrent hypertensive disorders) during pregnancy were more likely than normotensive women to subsequently develop diabetes, dyslipidemia, and hypertension. Women who remained normotensive while pregnant generally had lower BMI measurements than those who experienced PIH or preeclampsia.
Conclusion
Hypertensive disorders commonly develop during pregnancy. It is important to diagnose and classify PIH during routine prenatal visits. Once the diagnosis is made, patients must be monitored closely for increasing blood pressure or development of preeclampsia. Urine protein testing is a key clinical test to detect preeclampsia, and positive findings on a random urine protein dipstick should be confirmed and quantified with a 24-hour urine collection.
In addition to undergoing frequent blood pressure measurements and urine protein tests, patients should be asked about signs and symptoms that suggest preeclampsia. Women with mild PIH can be managed as outpatients with prenatal visits at least weekly, followed by delivery at term. Severely hypertensive patients are managed in the hospital with antihypertensive medications and prompt delivery at 34 weeks’ gestation or beyond, should maternal or fetal distress become evident.