A newer surgical procedure being used at Morgan Stanley Children's Hospital of NewYork-Presbyterian is spinal stapling.34 This involves minimally invasive surgery to implant inch-long staples across the spinal growth plates, which can stop scoliosis from worsening, or even correct the curve.
Spinal fusion with instrumentation, though used in less than 5% of patients with AIS, is considered the definitive surgical treatment for scoliosis.6 Surgical correction is almost always deemed necessary in immature patients with curves greater than 45° and mature patients with curves greater than 50°.3,7,22 The fusion may involve posterior (and sometimes anterior) discectomy and/or bone grafting between the involved vertebrae to help the bones fuse together so that curves cannot progress. The instrumentation (rods, hooks, wires, and/or screws) is used simply to maintain the spine in the best possible position until the actual fusion occurs; this can take months to a year.2,5,7
Risks and benefits of spinal fusion must be thoroughly reviewed with each parent and patient. The reported neurologic injury and mortality rates are less than 1% and less than 0.02%, respectively, in patients with idiopathic scoliosis who undergo the surgery.7 There is an increased incidence of such concerns in patients with other types of scoliosis, given their comorbid issues.35
Alternative treatments such as physical therapy, yoga, massage, acupuncture, and chiropractic medicine do not put patients at risk, and some have found them beneficial.3
EDUCATION
Both patient and parent must be acquainted with the goal of scoliosis diagnosis and treatment: to prevent curve progression, altered body image, and, ultimately, morbidity. Screening, history, examination, and radiographs are important first steps, with the information gained determining when referral to a pediatric spine orthopedist/specialist (if possible) should be made. Once curves reach 25° to 30°, bracing can successfully prevent curve progression; it will not correct the scoliosis.7 Teens who are resistant or reluctant to wear their brace must be made to understand the consequences of not following the treatment regimen, and the clinician's encouragement is essential.
Patients should be encouraged to stay active, with special emphasis on flexibility. Generally, there is no contraindication regarding activities or sports, unless the patient has undergone a surgical procedure; in this case, the practitioner will determine the patient's optimal level of participation in physical activities.
Surgical treatment with fusion and instrumentation is the only proven scoliosis treatment to correct curves (fully or partially) and prevent progression.3,5,7 Curves that reach 50° without treatment in the fully mature individual may continue to worsen into adulthood.
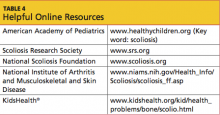
For patients with scoliosis having a possible familial and/or genetic component,2,3,7 there are several Web sites for patients and parents (see Table 4). Some of these address alternative therapy options.
CONCLUSION
Scoliosis is common, but the sequelae of idiopathic scoliosis can be minimized if the condition is diagnosed early and measures to prevent curve progression are initiated in a timely fashion. The key to diagnosing associated comorbid disorders and other related issues is to conduct a thorough patient and family history and complete physical examination. Timely radiographs are warranted in any patient with a positive finding. Ordering appropriate radiographs accurately is essential to facilitate patient care while reducing radiation exposure. Each practitioner must determine his or her level of comfort in managing patients with idiopathic scoliosis or immediately referring the patient once the diagnosis is made. Early referral is best in the primary care practice.