TABLE 1
Patient eligibility criteria for MTM programs17
| Multiple chronic diseases |
Programs must offer MTM services to patients who have at least 2 or 3 chronic diseases (at the plan’s discretion) and must target at least 4 of the following:
|
| Multiple covered drugs |
| Plans vary in the number of drugs patients must be prescribed to qualify, with thresholds ranging from 2 to 8. |
| Cost threshold |
| Patients must be expected to incur at least $3000 in annual Part D drug costs. |
| COPD, chronic obstructive pulmonary disease; MTM, medication therapy management. |
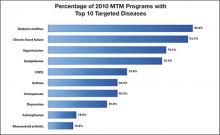
FIGURE
The top 10 diseases targeted by MTM programs in 2010 and the percentage of MTM programs that targeted these diseases17
COPD, chronic obstructive pulmonary disease; MTM, medication therapy management.
Reproduced with permission from Centers for Medicare and Medicaid Services. 2010 Medicare Part D Medication Therapy Management (MTM) Programs. https://www.cms.gov/PrescriptionDrugCovContra/ Downloads/MTMFactSheet_2010_06-2010_final.pdf. Published June 8, 2010. Accessed February 1, 2011.TABLE 2
Core elements of an MTM service model18
| Medication therapy review |
| Systematic review of the patient’s medications to assess and prioritize problems and create a plan to resolve them. |
| Personal medical record |
| Comprehensive record of the patient’s prescription and nonprescription medications, herbal agents, and nutritional supplements. The record is kept and updated by the patient, brought to appointments in different settings, and used by the patient in medication self-management. |
| Medication-related action plan |
| List of actions for the patient to use in self-management. The plan is developed collaboratively by the patient and pharmacist and used to track progress toward achieving specific goals. |
| Intervention and/or referral |
| The pharmacist intervenes or refers the patient to another health professional to address medication-related problems. |
| Documentation and follow-up |
| The pharmacist documents all MTM services and interventions— ideally, electronically. Follow-up or a referral to a different care setting is scheduled based on the patient’s needs. |
| MTM, medication therapy management. |
MTM services in pharmacy practice
MTM services are becoming well established in pharmacy practice. According to an annual survey conducted by the American Pharmacists Association, 72% of pharmacist respondents were offering MTM services in 2009, and about one-third of the rest planned to offer the services soon.19 About 84% of payer respondents (mostly health maintenance organizations, managed care insurers, and prescription benefit management plans) were offering MTM services. Contracted pharmacists provided about two-thirds of MTM care, with in-house pharmacists and contracted MTM organizations providing substantial amounts of services, and nurses and physicians providing a small proportion.19-20 MTM services are not restricted to Medicare patients, but are increasingly being offered by managed care organizations and fee-for-service plans.12,21 Some payers support pharmacist-provided MTM services as part of a broader multidisciplinary disease management program.20
Community pharmacists wishing to offer MTM services have several potential business models. Although they can contract directly with Medicare Part D insurers, it can be difficult and time-consuming to develop these individual contracts. Many insurers are not yet equipped to deal efficiently with pharmacists wishing to initiate this type of arrangement, and insurers are only slowly making the shift toward regarding pharmacists as providers.
A second option is to contract with an MTM intermediary company that links payers with pharmacists. These companies can be approached via their Web sites.12 Their services make it unnecessary for pharmacists to contract with different payers, find patients, or establish new billing systems. The American Society of Consultant Pharmacists offers a program through its Web site (http://www.ascp.org). Known as the MTM Provider Partners Program, it is a pathway for its members to enter the MTM world.
A third option is for pharmacists to provide patients with MTM services and then bill payers—so-called blind billing. Bills for patients covered by Medicare can be submitted using the CMS-1500 form available from the Web site of the Centers for Medicare and Medicaid Services, http://www.cms.gov. Assistance with billing codes is available from the Pharmacist Services Technical Advisory Coalition, http://www.pstac.org. It should be noted that although submission of these claims to various payers is becoming more standardized, there is no guarantee of payment with blind billing. Pharmacists may be reluctant to provide complex, time-consuming MTM services in the absence of such a guarantee. Providing MTM directly to patients in a fee-for-service manner is another option being explored in a few pharmacies.
Inconsistent documentation requirements and reimbursement policies among payers are barriers to community pharmacists’ adoption of MTMs.20 Other barriers to adoption of MTMs, or to their most effective use, include a lack of pharmacists’ time, staffing issues, difficulty forming collaborative relationships with physicians, poor patient mobility and low health literacy, a lack of medical information, and difficulty motivating patients to engage in the programs.15,20-23 It can be challenging to persuade patients of the value of a commitment to time-consuming MTM care, but once they have tried it, many become enthusiastic participants. As the following case study illustrates, use of the various components of the MTM model can help give patients with diabetes and multiple other illnesses a sense of ownership and control.