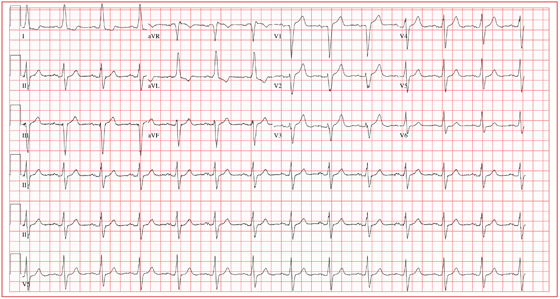
Answer
This ECG demonstrates normal sinus rhythm with left-axis deviation and left ventricular hypertrophy with QRS widening and repolarization abnormality, with no evidence of ischemia. Left-axis deviation is defined by an R-wave axis of less than –30° and is determined by examining leads III, aVF, and II. If leads III, aVF, and II are all negative, left-axis deviation is present. In this example, leads III and aVF are negative, while lead II is isoelectric or slightly negative.
Left ventricular hypertrophy is defined by high voltages in the limb leads (R wave in lead I plus S wave in lead III ≥ 25 mm) or in the precordial leads (S wave in V1 plus R wave in V5 or V6 ≥ 35 mm). The QRS duration, measured from the first deflection of the QRS from baseline to its return to baseline, is normal if ≤ 100 ms (0.10 sec). In this example, the QRS is widened (130 ms) in the absence of a bundle branch block. The delayed depolarization of both ventricles in the presence of left ventricular hypertrophy results in delayed repolarization—hence the repolarization abnormality.
This patient underwent cardiac catheterization, which revealed extensive three-vessel coronary artery disease with 99% stenosis of the proximal left anterior descending coronary artery. This case illustrates that severe coronary artery disease can present without ECG evidence of ischemia, particularly in women and in patients with diabetes.