For many patients, an AV fistula is created surgically when the eGFR falls to 15 mL/min/1.73 m2. Fistula placement in preparation for the initiation of hemodialysis is important to reduce the need for hemodialysis catheters, which are associated with higher risk for infection and poorer outcomes.33
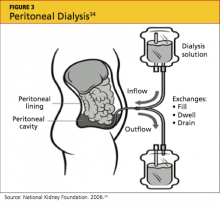
Peritoneal Dialysis
Peritoneal dialysis (PD) filters out uremic toxins and normalizes the metabolic and electrolyte derangements by using the patient’s peritoneal membrane as a filter. Dialysate is instilled through a catheter into the peritoneal cavity where it is allowed to dwell, often for four to six hours (see Figure 334). Exchanges can be performed three to four times per day (allowing six to eight hours of dwell time per exchange for the dialysate), or by way of a cycler at night.35,36
Performing exchanges by way of a cycler requires the patient to be connected via the PD catheter for eight hours; thus the advantage of performing the exchange during sleep. The cycler has a soft, whooshing sound that many patients describe as “white noise” that does not disturb their sleep.
The principal advantage of peritoneal dialysis is extended survival of the patient.37-39 PD also allows the patient a more liberal diet. Although PD must be performed every day, exchanges can be adjusted to the patient’s timing preference. PD reduces cost and time, since the patient need not travel to a dialysis center. PD also preserves residual renal function,39 which is associated with a survival benefit and contributes to the patient’s overall health and well-being. The use of PD requires a committed, competent patient in a clean home environment.
This intervention may not be suitable for patients with a history of abdominal surgeries. However, as a therapy considered gentler than hemodialysis, PD is an excellent choice for the patient with congestive heart failure.40 The PD catheter is not placed until two to four weeks before it will be needed.41
Kidney Transplantation
Last, but certainly not least, is transplant. As entire books have been written on this modality, only the highlights will be addressed here.42 Survival rates following transplantation are reported to exceed those associated with any other treatment modality, even when controlling for comorbidities and patient selection bias.43 A patient can receive a kidney from either a living or a deceased donor. Apart from the perioperative risks associated with transplantation surgery, long-term surgical or medical problems are not common for the living kidney donor.44-46
Since 2002, as a result of a policy change from the United Network for Organ Sharing (UNOS),47 the donor pool has been expanded by including kidneys from what are commonly referred to as extended criteria donors: those who are older than 60, or who are 50 to 59 and have two of the following factors: cerebrovascular accident as the cause of death; preexisting hypertension; or an SCr level exceeding 1.5 mg/dL. These kidneys may be given to any recipients but are primarily used for those age 50 or older.47
Graft survival is statistically shorter in a cadaver kidney than in a living donor kidney.48 However, the larger problem is the long wait time for a cadaver transplant—seven to eight years (or possibly longer) for some centers and some blood types.49 A patient can be referred to a transplant center when the eGFR falls below 25 mL/min/1.73 m2; he or she will then be actively listed for transplant when eGFR reaches 20 mL/min/1.73 m2 or lower.
Early referral for transplant listing buys the patient time before dialysis becomes essential. Patients can receive preemptive transplants (ie, transplantation before dialysis is initiated); these are becoming increasingly popular because they generally extend survival for the recipient.50,51
UNOS (www.unos.org) has set few limits on transplant recipients: patients are required to undergo an extensive medical work-up, but there are no upper age limits (although some centers do set their own) and usually no limits on patients infected with HIV, hepatitis B, or hepatitis C (although there may be separate listing requirements). Patients who are not US citizens are not denied.
Because more than 100,000 patients are currently on the wait list, domino kidney transplants are now being offered at many centers.52-54 These organ exchanges involve altruistic donors who do not match their targeted kidney recipients. Since publication of the first article describing this procedure at Johns Hopkins Medical Center,53 there have been two-way, three-way, and up to 32-way domino transplants. However, patients wishing to engage in this type of trade require a donor; not every patient has access to an altruistic donor.
CKD PATIENT EDUCATION
When Congress passed the Medicare Improvements for Patients and Providers Act of 2008,55 a component little noted outside the nephrology community was the offer of kidney disease education (KDE) classes to Medicare-eligible patients with CKD 4.56-58 Medicare patients with an eGFR of 15 to 30 mL/min/1.73 m2 are eligible to attend KDE classes presented by a physician, an NP, a PA, or a clinical nurse specialist. Medicare will reimburse for six hours of education.