This groundbreaking educational benefit, the first such program paid for by Medicare, was championed by the National Kidney Foundation and other nephrology groups. Many nephrology practices now offer these classes to all their CKD patients, regardless of health insurance status. Instructors educate patients on the choices of renal replacement therapy and help patients select their best option.
KDE classes can be conducted in the office setting or at the patient’s home, and they can be billed on the same day as an evaluation and management (E/M) visit.56,57 This may help explain why, in 2010, gerontologists billed for more home KDE classes than did nephrologists.58
FUTURE TRENDS AND ONGOING TRIALS
The overarching goal of therapy for CKD patients is to diagnose accurately and treat effectively in order to slow or prevent progression to end-stage renal disease (ESRD). Following is a brief review of a selection of new diagnostic tools and therapeutic interventions that may impact the management of CKD in the coming years.
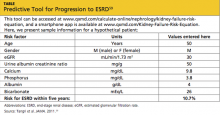
The QxMD Kidney Failure Risk Equation is a newly developed, well-validated predictive model that offers relatively accurate prediction of a patient’s likelihood of progression to ESRD, based on age, sex, eGFR, and levels of albuminuria, SCr, serum phosphorus, serum bicarbonate, and serum albumin59 (see table59). This tool can be accessed online at www.qxmd.com/calculate-online/nephrology/kidney-failure-risk-equation.
Increased awareness of the role that phosphorus plays in the development of vascular calcifications has led to an emphasis on earlier, more aggressive control of dietary phosphorus. Historically, dietary phosphorus control and phosphorus binders were recommended only when the patient’s serum phosphorus exceeded normal limits. Dietary phosphorus control may now be advised as early as CKD 3, based on the understanding that phosphorus is a key component in driving the development of vascular calcifications—which in turn contribute to the high incidence of cardiovascular disease in patients with CKD.60
Bardoxolone is a new medication developed for treatment of diabetic nephropathy.61,62 It works by inhibiting proinflammatory mediators and moderating the effects of oxidative stress, thus interrupting the cascade of inflammation and cellular injury that result in diabetic nephropathy.62 Early clinical trials examining this agent have shown promise in terms of raising eGFR and reducing serum creatinine, but tolerability and toxicity profiles have been an issue.61 Additionally, some reduction in serum creatinine may have been attributable to weight loss as opposed to true improvement of renal function.62
Data have recently been released regarding the use of the herb silymarin for treatment of patients with macroalbuminuria related to diabetic nephropathy. Results from a small (n = 60), randomized, nonblinded clinical trial by Fallahzadeh et al63 indicate that silymarin decreases proteinuria when used in combination with an ACE inhibitor or an angiotensin receptor blocker (ARB). Silymarin, an extract from milk thistle, has been used medicinally for centuries for its antioxidant, anti-inflammatory, and antiviral properties in those with liver “ailments.” In this clinical trial, silymarin was well tolerated and associated with a reduction in pro-inflammatory markers.63
AST-120 is another agent intended to slow progression of CKD. It promotes intestinal adsorption and fecal excretion of the uremic toxin indoxyl sulfate.64 A recently published study demonstrated an association between use of AST-120 and a delay in required initiation of hemodialysis, but no survival benefit.65 This was a nonrandomized trial, and previous research showed no effect of AST-120 on progression of CKD.66 However, patients close to requiring dialysis are likely to welcome a means to delay it.
A growing body of evidence suggests that reversal of CKD-associated acidemia by administering sodium bicarbonate may actually forestall progression of CKD.67 However, treatment with sodium bicarbonate can lead to complications of hypertension and fluid volume overload. In one study, patients at risk for these complications derived equivalent benefit by increasing dietary fruit and vegetable intake to reduce renal acid load.68 However, providers must be mindful of patients’ serum potassium levels, especially patients who are taking an ACE inhibitor or an ARB.
The Provider’s Current Role
Despite the hope offered by new and novel therapies, the mainstay of treatment for CKD continues to be aggressive management of diabetes, hypertension, and the cardiovascular risk profile. As a result of vigorous preventive strategies to address the cardiovascular risks inherent in this patient population, the patient with type 2 diabetes is now more likely to progress to ESRD than to die of a cardiovascular event.69
The well-informed clinician can be instrumental in providing evidence-based medical therapy and excellent patient education from the time of initial CKD diagnosis through CKD 5.
PATIENT OUTCOME
The case patient was started on injections of epoietin alfa for her anemia. She attended KDE classes led by an advanced practitioner in her nephrology group and decided to undergo peritoneal dialysis, since it would allow her to maintain her travel schedule. When last heard from, the patient was preparing for a trip to see the Great Barrier Reef in Australia.